- Gonococcal antimicrobial resistance to ceftriaxone remains low in the United States. Antimicrobial resistance to azithromycin has increased in recent years
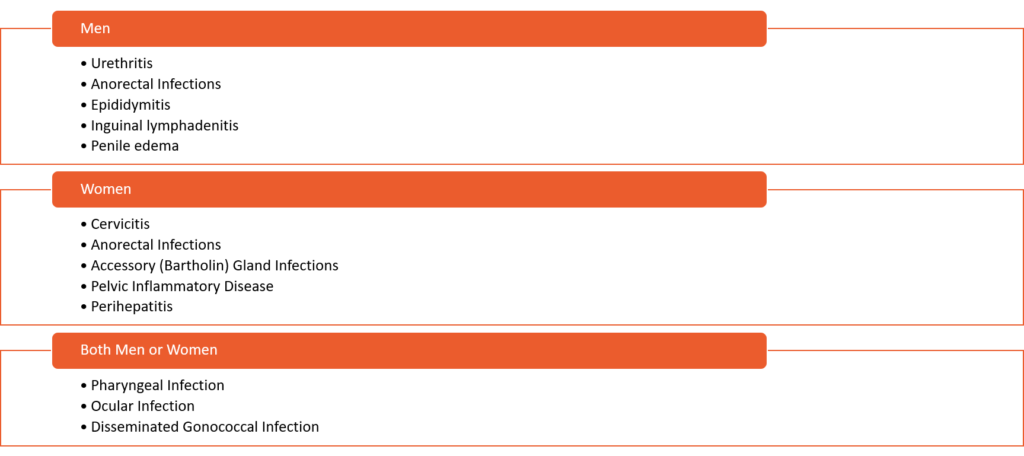
- Neisseria gonorrhoeae can cause a wide array of urogenital, pharyngeal, and rectal symptoms as well as serious complications, such as pelvic inflammatory disease, tubal infertility, ectopic pregnancy, neonatal conjunctivitis, and rarely, disseminated infection
- NAAT is the preferred test for screening/diagnosing gonorrhea in both men and women
- Cultures can used when the concern for antimicrobial resistance arises
- A test-of-cure is not recommended after treatment of uncomplicated infections of:
- Cervix
- Urethra
- Rectum
- A test-of-cure should be performed:
- In all persons at 7 to 14 days following the treatment of pharyngeal gonorrhea
Clinical Manifestations
In 2019, a total of 616,392 cases of Neisseria gonorrhoeae (gonorrhea) were reported in the United States, making gonorrhea the second highest reported bacterial STI
Gonorrheal Infection Screening
- WOMEN
- Routine screening for gonorrhea is recommended for all sexually active women younger than 25 years of age.
- Sexually active women age 25 years and older should have screening for gonorrhea if they are at increased risk
- Screening for pharyngeal and rectal gonorrhea screening can be considered in females based on reported sexual activities and exposure through shared clinical decision-making.
- WOMEN WHO HAVE SEX WITH WOMEN (WSW) AND WOMEN WHO HAVE SEX WITH WOMEN AND MEN (WSWM)
- Gonorrhea screening recommendations for women who have sex only with women (WSW) and women who have sex with women and men (WSWM) are the same as outlined above for women who have sex with men.
- PREGNANT WOMEN
- Routine screening for gonorrhea should be performed on all pregnant women younger than 25 years of age and in older pregnant women if at increased risk for gonococcal infection
- Retest for gonorrhea should be done during the 3rd trimester for women under 25 years of age or those with increased risk for acquiring gonorrhea during the pregnancy.
- MEN WHO HAVE SEX ONLY WITH WOMEN
- For men who have sex only with women, routine screening for gonococcal infection is not recommended.
- MEN WHO HAVE SEX WITH MEN (MSM)
- All sexually active MSM should undergo screening for gonorrhea at least annually.
- Screening should consist of testing at sites of sexual contact (urethra, rectum, pharynx). The preferred tests (self-collected or provider-collected) are urine NAAT, rectal NAAT, and pharyngeal NAAT.
- More frequent screening at 3- to 6-month intervals is indicated for men who have sex with men if they have increased risk
- TRANSGENDER AND GENDER DIVERSE PERSONS
- Routine gonorrhea screening should be adapted based on the individual’s anatomy.
- For example, all transgender men and gender diverse persons who have a cervix should have the same screening for gonorrhea as cisgender women who have sex with men
- Consider screening at the pharyngeal and rectal sites based on reported sexual activity and exposures.
- PERSONS WITH HIV
- All persons with HIV who are sexually active should have screening for gonorrhea at the initial HIV evaluation visit and at least annually thereafter.
- Some individuals may require more frequent screening depending on their sexual activity and local epidemiology for their region.
- PERSONS IN CORRECTIONAL FACILITIES
- Routine opt-out screening for gonococcal infection should be offered at intake upon entering a correctional facility for women 35 years of age and younger and for men younger than 30 years of age.
