- Chlamydia is the most common reportable bacterial STI in the United States, with 1,808,703 reported cases in 2019
- From 2015-2019, there was an 18% increase in reported cases of chlamydia in the United States
- Rates of C. trachomatis transmission between sex partners is approximately 55%, with a per-act transmission of urogenital infection of about 10%
- Factors associated with the acquisition of chlamydial infection include:
- A previous or coexisting STI
- New or multiple sex partners
- A new sex partner
- More than one partner
- A sex partner who is having sex with other partners at the same time
- A sex partner who has an STI
- Inconsistent condom use
- History of incarceration
- Exchanging sex for money or drugs
Chlamydia trachomatis is an obligate intracellular bacterium with a cell wall and ribosomes similar to those of gram-negative organisms
- The species C. trachomatis, which exclusively infects humans, can cause
- (1) trachoma in persons of all ages
- (2) anogenital infections, lymphogranuloma venereum (LGV), and conjunctivitis in adolescents and adults
- (3) conjunctivitis and pneumonia in neonates
- C. trachomatis typically infects columnar epithelial cells at mucosal sites, often becoming a chronic infection that may last months or even longer than a year if untreated
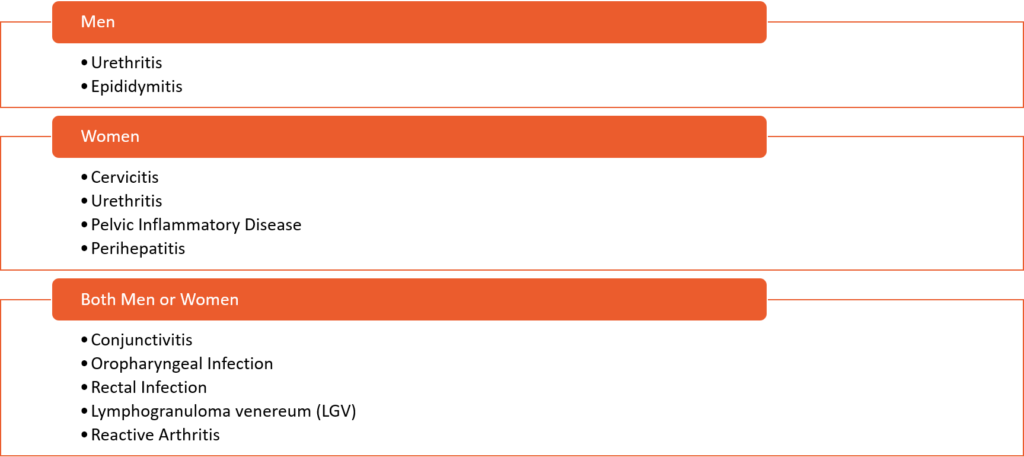
Clinical Manifestations
Chlamydial Infection Screening
- WOMEN WHO HAVE SEX WITH MEN
- All sexually active women younger than 25 years of age should undergo annual screening.
- (1) the incidence of chlamydial infection is highest in women 15-25 years of age
- (2) chlamydia infection is typically asymptomatic in women
- (3) untreated chlamydial infection in women can cause severe health and reproductive complications.
- For young women, more frequent screening (at 3- to 6-month intervals) may be indicated based on their sexual activity
- Women 25 years of age and older should undergo routine screening if they are considered to have increased risk for chlamydial infection (e.g. those who have a new sex partner, more than one sex partner, a sex partner with concurrent partners, or a sex partner who has an STI).
- Screening for rectal chlamydia (based on history of receptive anal or oral sex) should be considered through a shared clinical decision-making process between the woman and the health care provider.
- All sexually active women younger than 25 years of age should undergo annual screening.
- WOMEN WHO HAVE SEX WITH WOMEN
- Screening should be offered per the screening guidelines for sexually active women who have sex with men
- PREGNANT WOMEN
- At the first prenatal visit, screen all pregnant women younger than 25 years of age
- At the first prenatal visit, screen all pregnant women 25 years of age and older who have increased risk for chlamydial infection
- Retest for chlamydial infection during the third trimester in all women younger than 25 years of age and in women older than 25 years of age who have an increased risk of acquiring chlamydial infection
- Pregnant women diagnosed with chlamydia should have a test-of-cure 4 weeks after completing treatment and repeat testing for chlamydia within 3 months after completing treatment
- MEN WHO HAVE SEX ONLY WITH WOMEN
- Routine screening for chlamydial infection is not recommended for sexually active men who have sex only with women
- Targeted screening for men should be considered if resources permit, the community prevalence is high, and such screening does not hinder chlamydia screening efforts for women.
- Screening can be considered in sexually active young men in high chlamydia prevalence settings, including adolescent clinics, correctional facilities, STI clinics, or sexual health clinics
- MEN WHO HAVE SEX WITH MEN
- All sexually active men who have sex with men should undergo screening at least annually
- Screening should consist of testing urethral and rectal sites for those who report exposures at these sites during sexual activity, regardless of condom use during sexual activity
- Routine testing of oropharyngeal testing for chlamydia infection is not recommended
- More frequent screening at 3- to 6-month intervals is indicated for men who have sex with men if they have increased risk (e.g. persons taking HIV preexposure prophylaxis, individuals with HIV, persons with ongoing risk for acquiring chlamydia, and persons who have multiple sex partners or their sex partners have multiple partners).
- TRANSGENDER AND GENDER DIVERSE PERSONS
- Screening for chlamydial infection in transgender and gender diverse persons should be based on the person’s sexual practices, age, and genital anatomy.
- For example, if an individual is sexually active, younger than 25 years of age, has a cervix, and identifies as a transgender man or nonbinary, they should have annual chlamydial screening, similar to screening in cisgender women who have a cervix.
- Screening for transgender women who have undergone vaginoplasty surgery should include screening of the neovagina.
- The optimal method for neovagina chlamydial screening (vaginal swab versus urine) is not known
- Screening for chlamydia infection in transgender men who have undergone metoidioplasty surgery (with urethral lengthening), but not vaginectomy, should utilize a vaginal swab to detect cervical infection due to the low yield of urine testing in this post-surgical setting.
- PERSONS WITH HIV
- Screening for chlamydial infection is recommended for persons with HIV who are sexually active; the screening should take place at the initial evaluation and at least annually thereafter.
- More frequent screening (e.g. every 3 to 6 months) may be indicated for persons with HIV based on risk activity, persons on HIV preexposure prophylaxis (PrEP), and local prevalence of specific STIs.
- Testing samples should be obtained from the anatomic sites of sexual exposure
- CORRECTIONAL FACILITIES
- Routine opt-out screening for chlamydial infection screening of all sites of sexual activity (pharyngeal, urethral or vaginal, and rectal) should be offered during intake (or within 48 hours of intake) at correctional facilities for all females 35 years of age and younger and all males younger than 30 years of age
