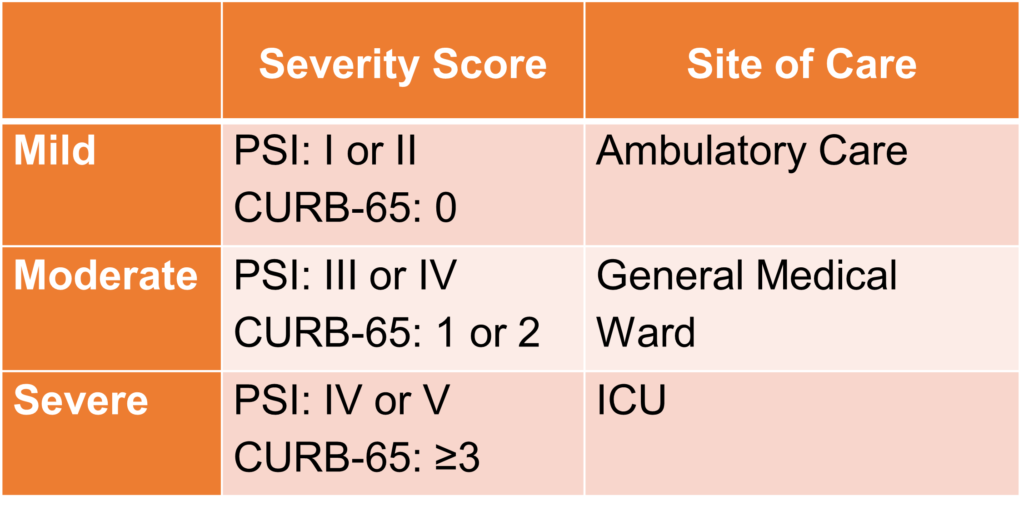
For patients with a working diagnosis of CAP, management relies on defining the severity of the illness to determine the most appropriate approach. The severity of illness is based on clinical judgment and can be supplemented by the use of severity scores such as the Pneumonia Severity Index (PSI) and CURB-65, in which PSI or PORT score is more preferred.
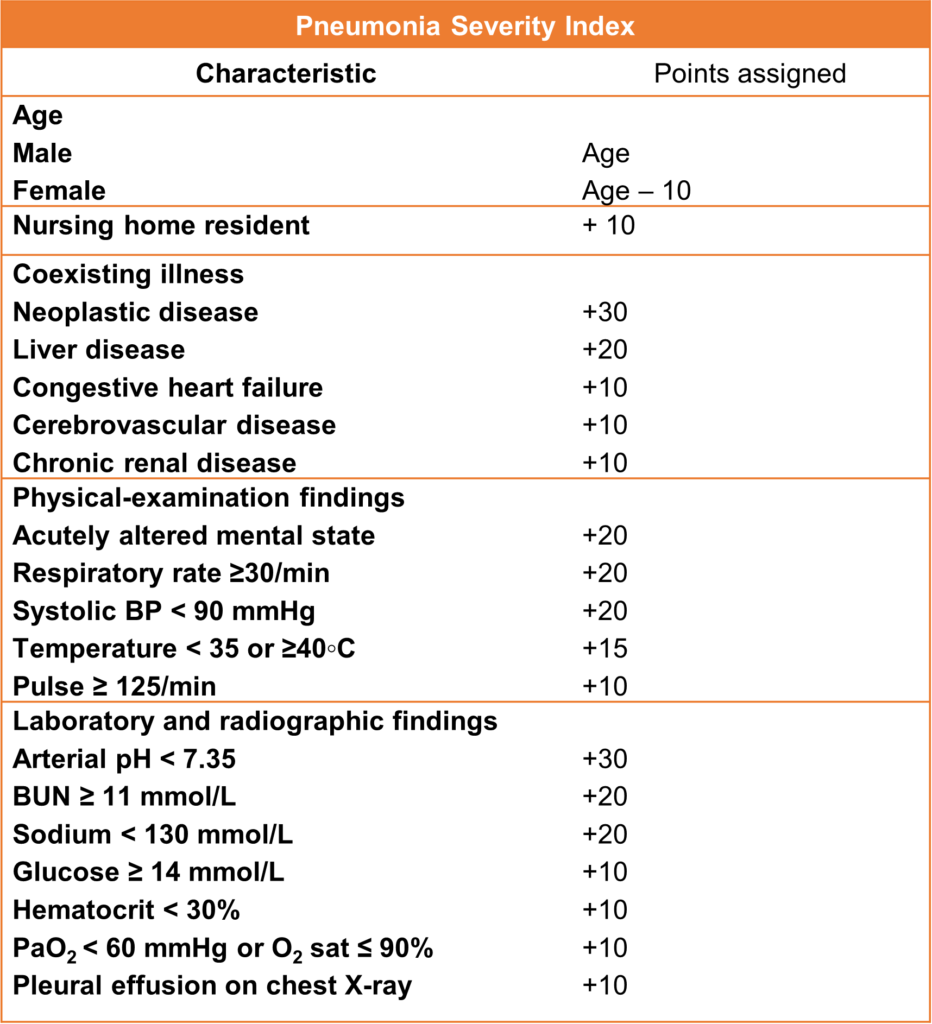
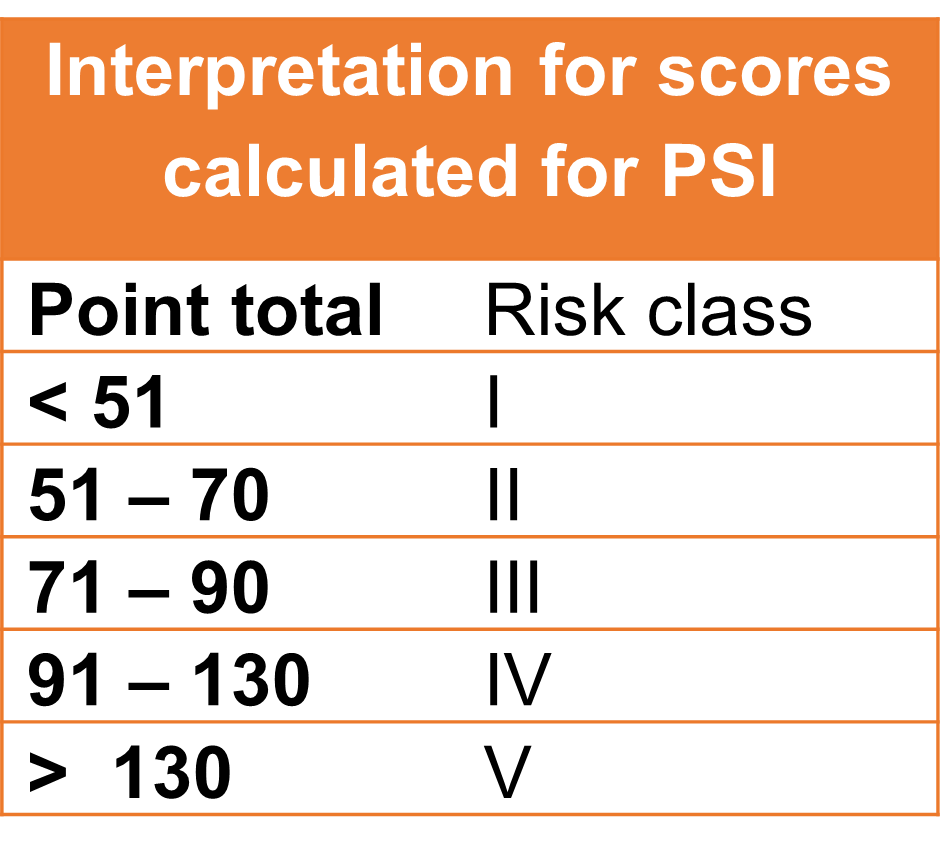
Pneumonia Severity Index / PSI or PORT Score
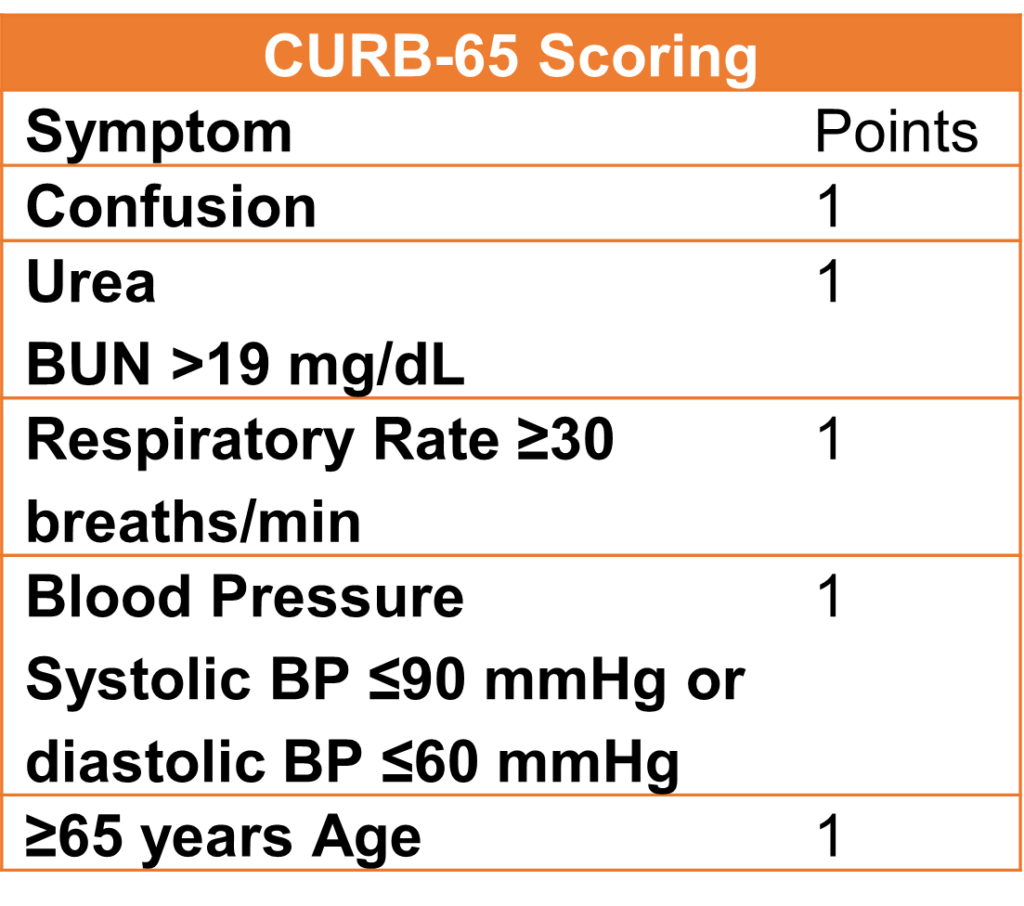
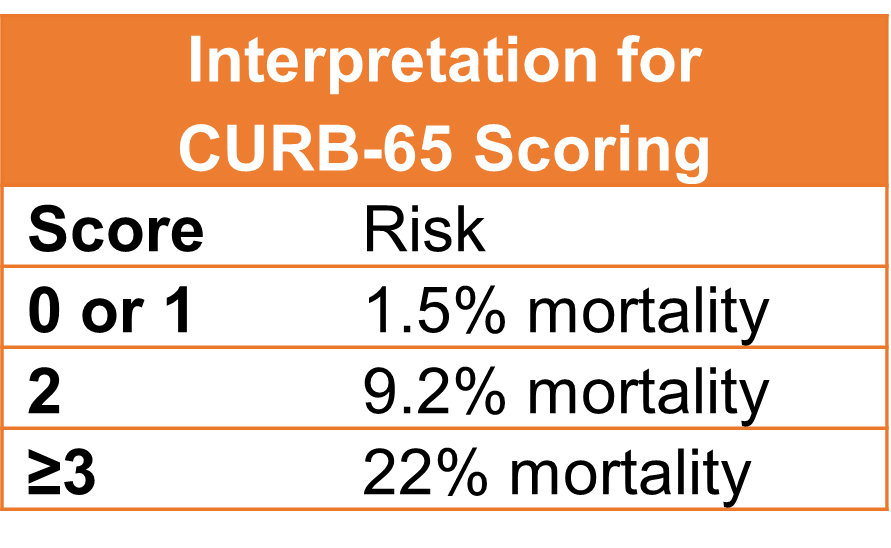
CURB-65 Scoring
CAP Initial Evaluation and Site of Care Based on Severity Assessments
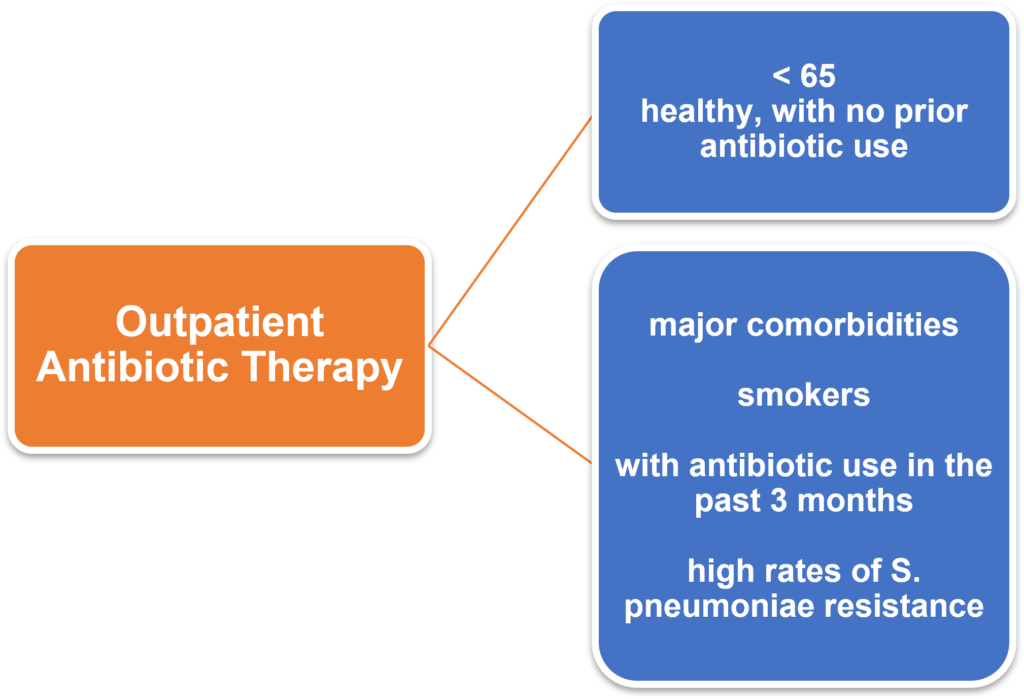
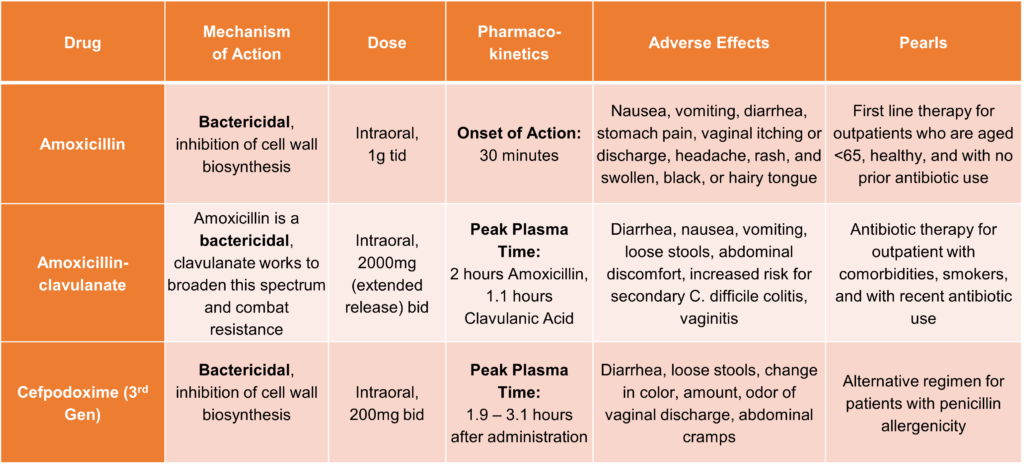
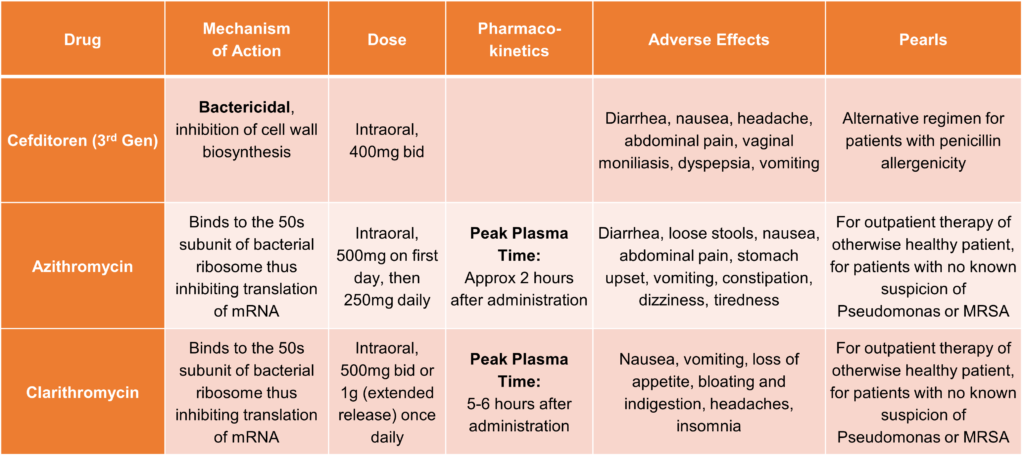
Empiric Antibiotic Therapy: Outpatient
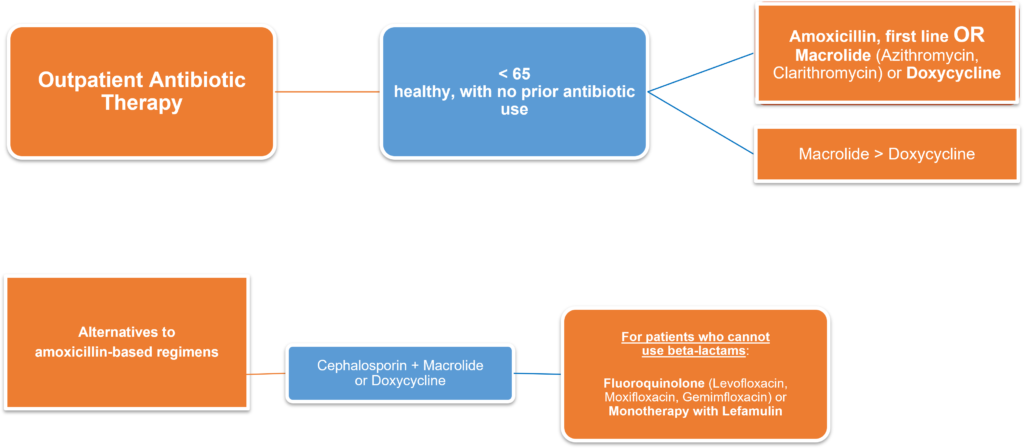
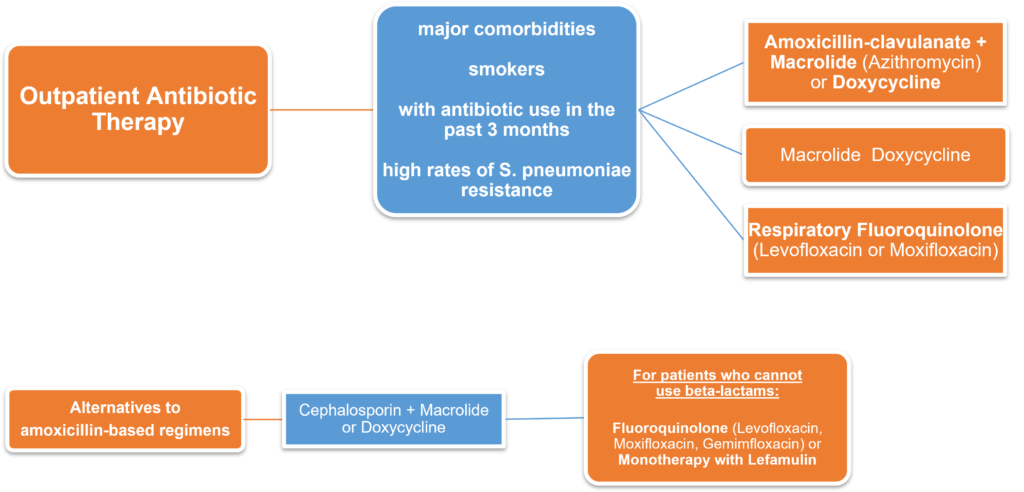
- Patients are often treated for 5 days.
- Ensure that all patients are responding positively to antibiotic therapy and remain afebrile for at least 48 hours before stopping antibiotics.
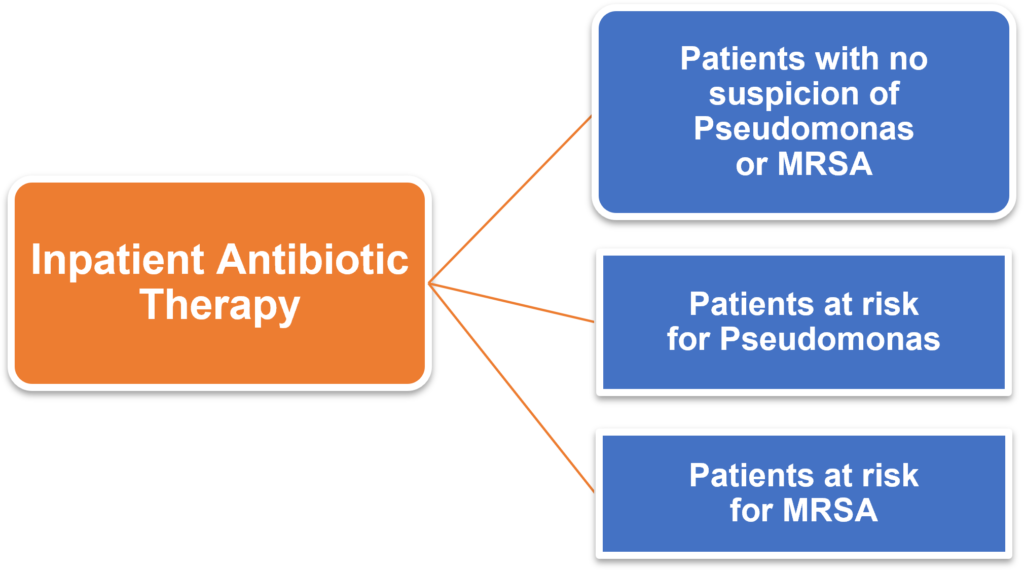
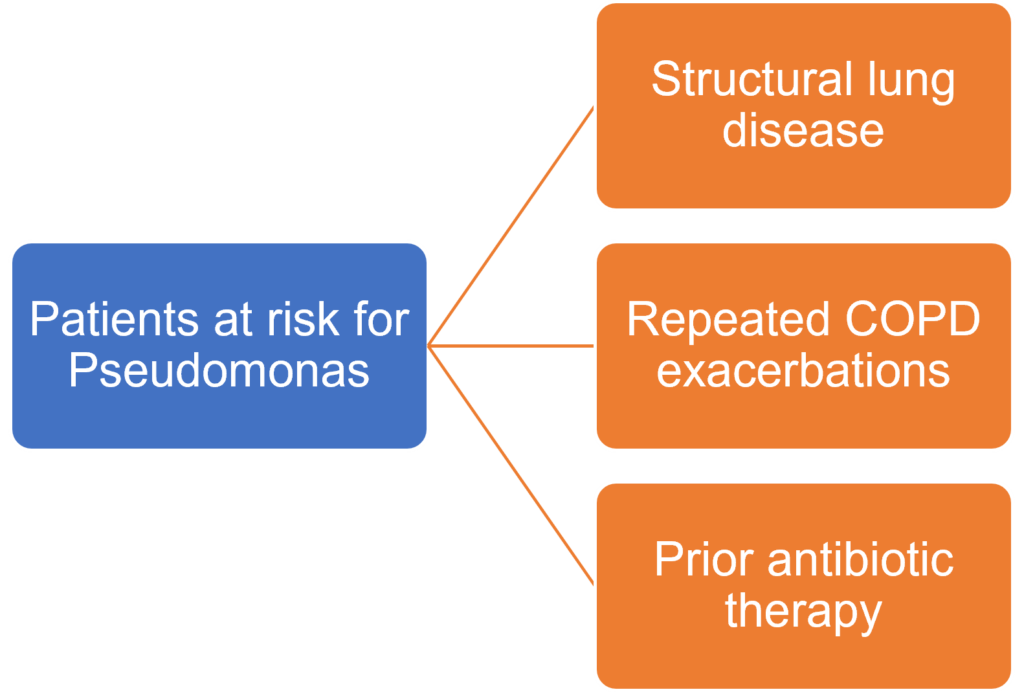
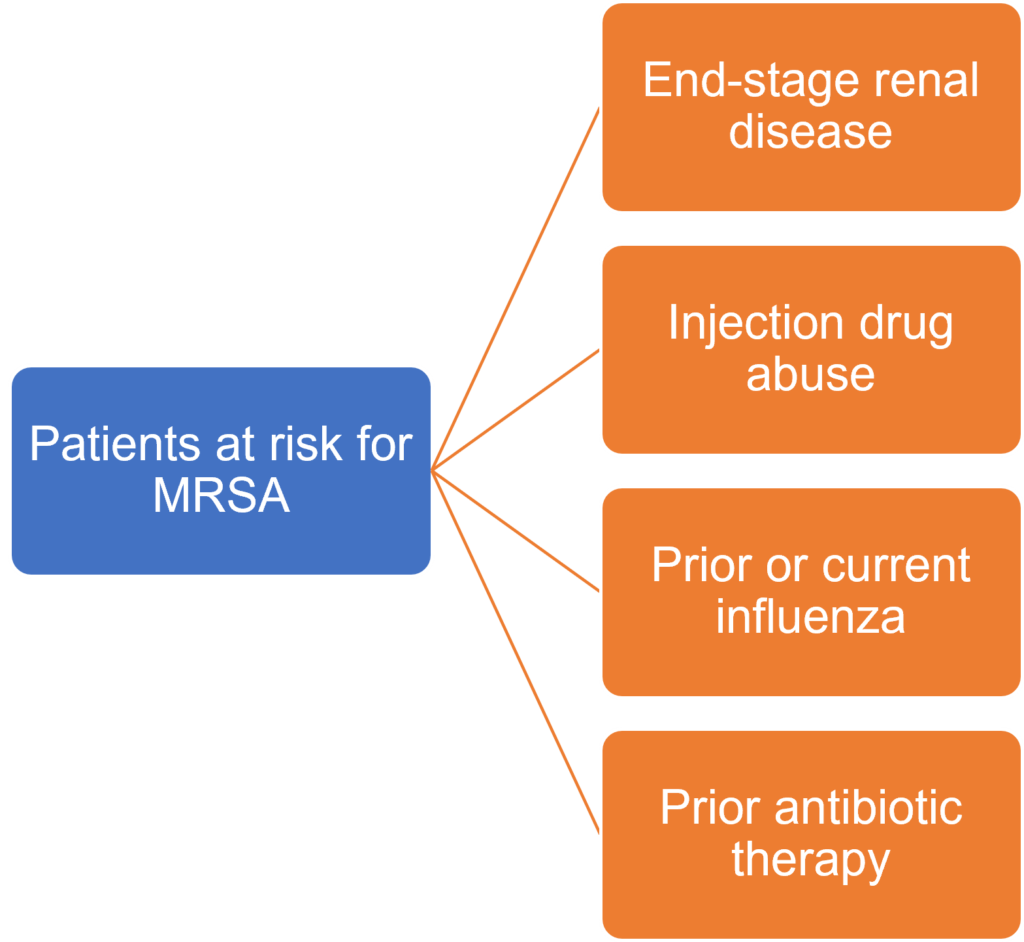
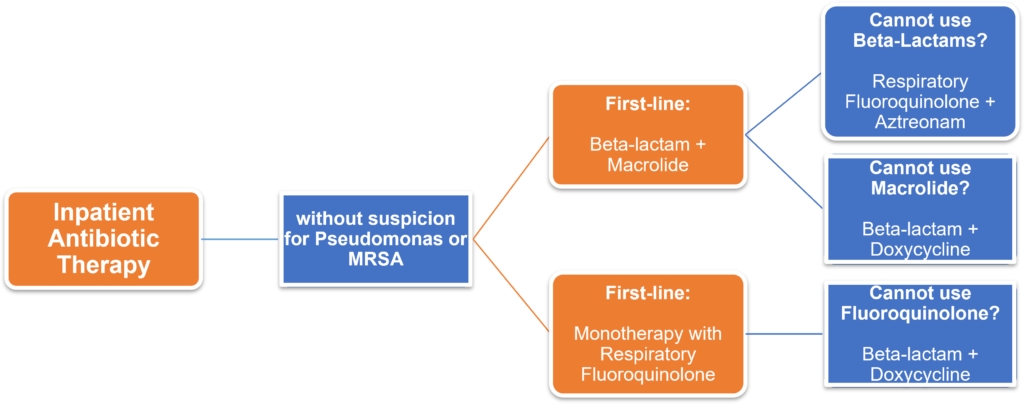
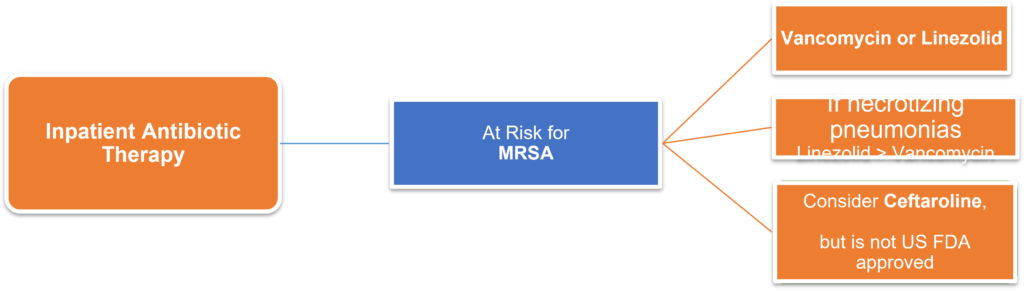
Empiric Antibiotic Therapy: Inpatient (Ward or ICU)
- First-line: Beta-lactam + Macrolide or Respiratory Fluoroquinolone
- Antibiotic therapy should be initiated within 4 to 8 hours of hospital arrival for patients with radiographically confirmed pneumonia and moderate to high levels of illness severity presentation.
- Identify risk factors to begin empiric antibiotic therapy.

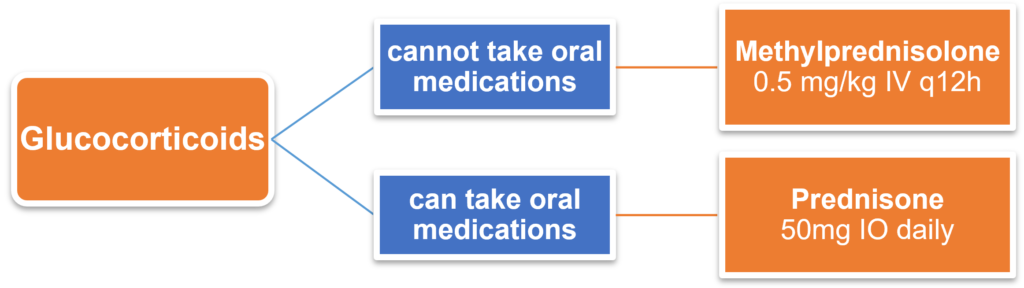
Adjunctive Glucocorticoids
- For patients with as septic shock with one or more of the following:
- Metabolic acidosis, arterial pH <7.3
- Lactate <4 mmol/L
- C-reactive protein > 150 mg/L
Factors Relevant to Initial Antibiotic Therapy
- Disposition
- Patients generally make clinical improvements within 48 – 72 hours. Further management is dictated by the patient’s response to initial empiric therapy. Make daily assessments on clinical response and improvements on cough, sputum production, dyspnea, and chest pain. Also assess for resolution of fever and normalization of heart rate, RR, and WBC count.
- Antibiotic Deescalation
- Tailor therapy to attack the pathogen. If not present, continue empiric antibiotic therapy until patient shows signs of improvements.
- Duration of Therapy
- This is often based on the patient’s response to therapy. All patients are generally treated for 48 hours to a minimum of 5 days and until they are afebrile and clinically stable.
- Mild infections – 5 – 7 days of therapy
- Severe infections or chronic comorbidities: 7 – 10 days of therapy
- Extended courses may be needed for immunocompromised patients, those with causative pathogen involvement, or those with complications.
- This is often based on the patient’s response to therapy. All patients are generally treated for 48 hours to a minimum of 5 days and until they are afebrile and clinically stable.
- Discharge
- Only recommended if patient is clinically stable, can take oral medications, has no other active medical problems, and has a safe environment for continued care.
- Criteria for clinical stability:
- Temperature ≤37.8◦C
- HR ≤100bpm
- RR ≤24brpm
- Systolic BP ≥90mmHg
- Arterial O2 Saturation ≥90% or pO2 ≥60 mmHg on room air
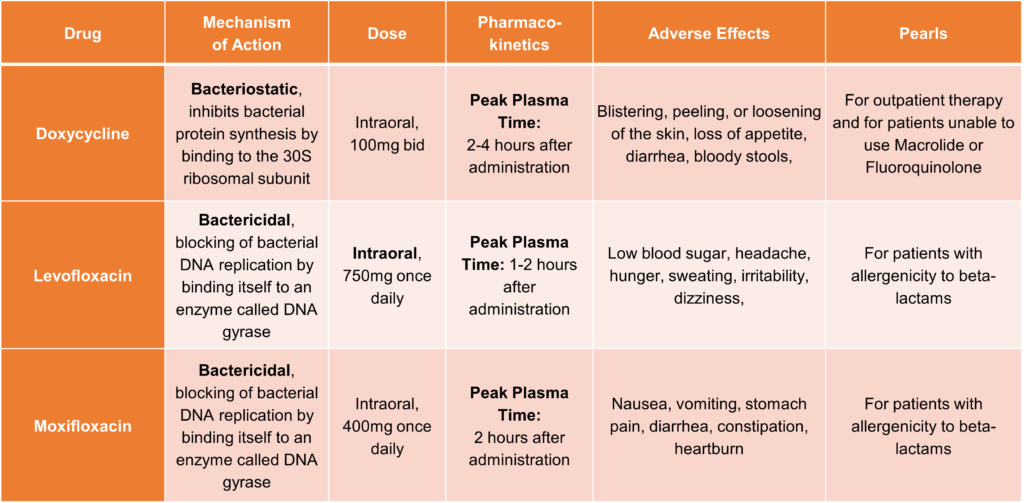
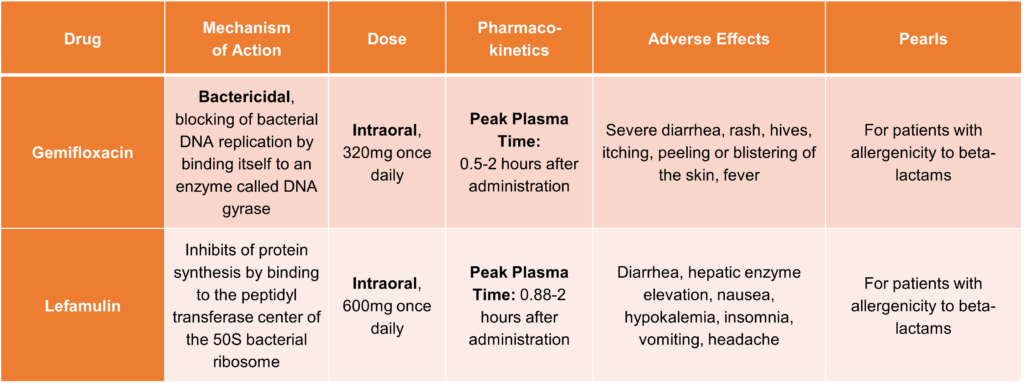
Antibiotic Therapy for CAP
References:
1. Ramirez, et al. Overview of Community-Acquired Pneumonia in Adults. 2021
