Succinylcholine
Mechanism of Action
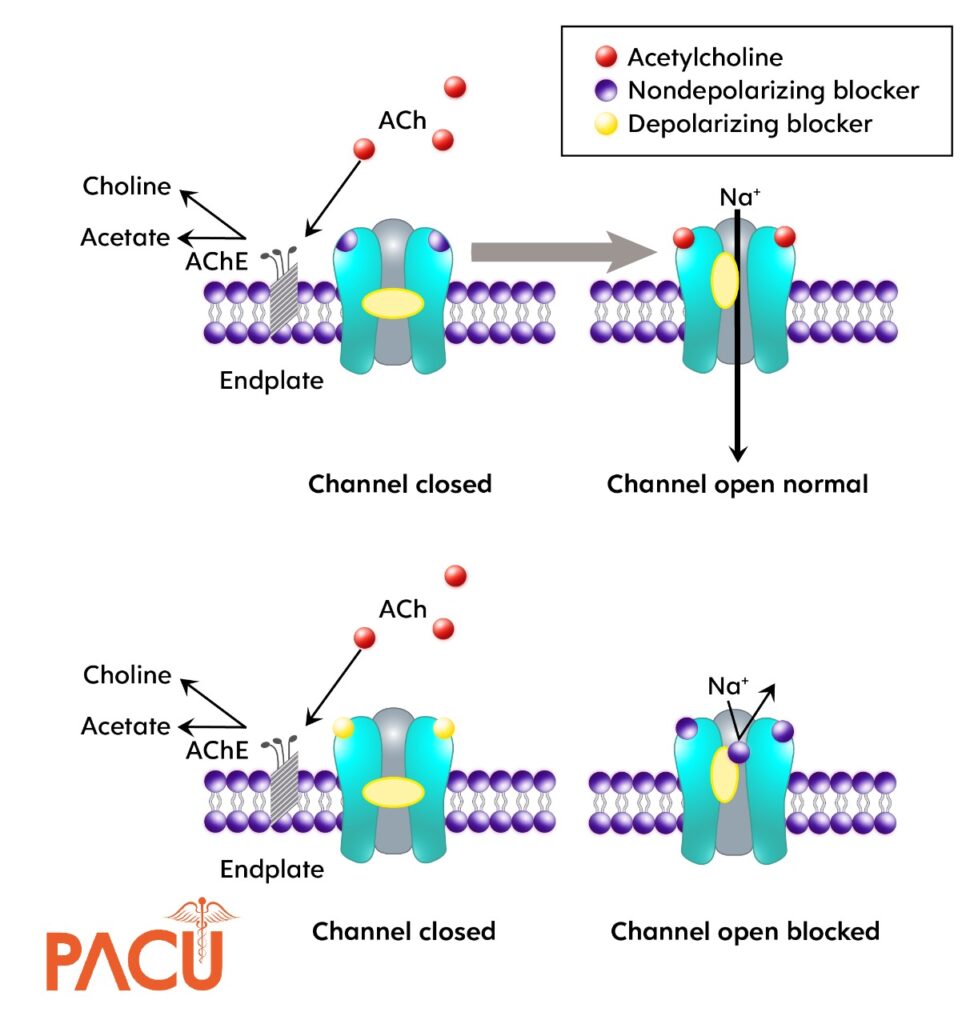
- Succinylcholine is a depolarizing neuromuscular blocker (NMBA) that resembles the structure of 2 molecules of acetylcholine.
- Only depolarizing NMBA in the United States
Succinylcholine binds to nicotinic acetylcholine receptors at the motor endplate and causes depolarizations and continuous stimulation to the endplate which inhibits repolarization
Dose
1 to 2 (commonly 1.5) mg/ kg total body weight IV
Lower doses have been studied (0.3-0.6 mg/kg), however, the onset of action with lower dosages isn’t ideal for emergent intubations such as RSI
3-4 mg/kg IM
Onset
IV: 10-50 seconds
IM: 3-4 minutes
Duration
- 3-10 minutes
Metabolism
- Rapidly hydrolyzed by plasma pseudocholinesterase to inactive metabolites
- Plasma cholinesterase activity may be diminished in patients with genetic abnormalities of plasma cholinesterase, malignant tumors, infections, burns, anemia, and decompensated heart disease.
- This is insignificant clinically as duration is extended by 15-20 minutes.
- Plasma cholinesterase activity may be diminished in patients with genetic abnormalities of plasma cholinesterase, malignant tumors, infections, burns, anemia, and decompensated heart disease.
Elimination
- Renal Excretion: 10%
Adverse effects
- Bradycardia
- Hyperkalemia
- Fasciculations
- ↑ intraocular pressure
- Transient ↑ ICP ~5-10 mmHg
- Malignant hyperthermia (rare)
Contraindications
- History of malignant hyperthermia in the patient or family
- Patients at high risk of severe hyperkalemia
- Burns, crush injuries, spinal cord injuries, strokes, and intraabdominal sepsis >5 days old
- Neuromuscular diseases, e.g., multiple sclerosis, amyotrophic lateral sclerosis, myasthenia gravis myopathies
- Allergy to class/drug
- spinal cord damage (1 week – 3 months old)
Pearls
Cholinesterase inhibitors (neostigmine) don’t reverse depolarization NMBAs and may prolong the duration of action of succinylcholine by promoting higher acetylcholine concentration at the nerve terminal.
Succinylcholine-induced depolarization could lead to an increase in serum potassium by 0.5 mEq/L.
While Succinylcholine leads to a transient increase in intraocular pressure and intracranial pressure, data has not confirmed that this leads to worse patient outcomes.
In theory, subsequent dosing of succinylcholine could lead to secondary block which could lead to SA nodal blockade and resultant bradycardia.
Bradycardia is more common in the pediatric population due to the vagal predominance in the autonomic nervous system.
Literature Review
| Author, year | Design/ sample size | Intervention & Comparison | Outcome |
|---|---|---|---|
| Guihard, 2019 | Noninferiority randomized clinical trial n=1248 | Succinylcholine ≥ 1.5 mg/kg vs Rocuronium ≥ 1.2 mg/kg | Successful first-attempt intubation was 455 of 610 (74.6%) in the rocuronium group vs 489 of 616 (79.4%) in the succinylcholine group, with a between-group difference of -4.8%, which did not meet criteria for noninferiority. |
| April 2018 | Prospective cohort study n= 4,275 | Succinylcholine ≥ 1 mg/kg vs Rocuronium ≥ 1.2 mg/kg | The first-pass intubation success rate was no difference between the agents with 87.0% with succinylcholine versus 87.5% with rocuronium (adjusted OR 0.9; 95% CI 0.6- 1.3 |
| Patanwala, 2016 | Retrospective cohort study n=233 | Succinylcholine (dosing not reported) vs Rocuronium (dosing not reported) | In the high-severity TBI patients, succinylcholine was associated with increased mortality compared with rocuronium (OR 4.10, 95% CI 1.18–14.12). |
| Watt, 2012 | Retrospective cohort study n=200 | Succinylcholine 1.7 ± 0.7 mg/kg vs Rocuronium 1.3 ± 0.4 mg/kg | After intubation, 77.5% (n=155) of patients were initiated on a sedative infusion of propofol (n=148) or midazolam (n=7). Mean time to post-intubation sedation was significantly greater with rocuronium compared to succinylcholine (27 min vs 15; p <0.001) |
Comments by ED Physician Attendings
| Pro’s | Con’s |
| ” I like the shorter duration of paralysis” | ” Can see hyper-K with CNS/spinal cord injury (>3 days), myopathies, burns (few days late), sepsis, critical illness, and occasionally with severe traumatic injury acutely due to succinic acid mechanism. Avoid sux when possible in pediatric populations (<8) “ |
Rocuronium
Mechanism of Action
- Rocuronium is a nondepolarizing NMBA that acts as a competitive inhibitors of acetylcholine (ACh) receptors.
- Nondepolarizing NMBAs bind to the ACh receptor without causing a conformational change which would tradionally allow passage of sodium ions.
- Rocuronium is monoquaternary steroid analogue of vecuronium designed to provide a rapid onset of action
Dose
- 1 to 1.2 (commonly 1) mg/ kg total body weight IV
- In obese patients ideal body weight (IBW) or total body weight (TBW) may be used
Lower doses have been studied (<1 mg/kg), however, the onset of action with lower dosages isn’t ideal for emergent intubations such as RSI.
Onset
- IV: 45-90 seconds
- Larger doses lead to quicker onset of action
Duration
- 30-90 minutes
- Larger doses leads to more prolonged duration of action
Metabolism
- Minimally hepatically
Elimination
- Renal Excretion: Feces (31%); urine (26%)
Adverse effects
- Very few reported, but possible increased peripheral vascular resistance (abdominal aortic surgery)
Contraindications
- Contraindications
- Allergy to class/drug
Pearls
The main problem with high dose nondepolarizing neuromuscular blocking agents is prolonged recovery time
If a patient needs to have frequent neurological assessments soon after intubation, reversal of rocuronium could be considered with a neostigmine + atropine or sugammadex.
Have post-intubation sedation plan set prior to intubation to minimized awake paralysis
Literature Review
| Author, year | Design/ sample size | Intervention & Comparison | Outcome |
|---|---|---|---|
| Guihard, 2019 | Noninferiority randomized clinical trial n=1248 | Succinylcholine ≥ 1.5 mg/kg vs Rocuronium ≥ 1.2 mg/kg | Successful first-attempt intubation was 455 of 610 (74.6%) in the rocuronium group vs 489 of 616 (79.4%) in the succinylcholine group, with a between-group difference of -4.8% (1-sided 97.5% CI, -9% to ∞), which did not meet criteria for noninferiority. |
| April, 2018 | Prospective cohort study n= 4,275 | Succinylcholine ≥ 1 mg/kg vs Rocuronium ≥ 1.2 mg/kg | The first-pass intubation success rate was no different between the agents with 87.0% with succinylcholine versus 87.5% with rocuronium (adjusted OR 0.9; 95% CI 0.6- 1.3 |
| Patanwala, 2016 | Retrospective cohort study n=233 | Succinylcholine (dosing not reported) vs Rocuronium (dosing not reported) | In the high-severity TBI patients, succinylcholine was associated with increased mortality compared with rocuronium (OR 4.10, 95% CI 1.18–14.12). |
| Watt, 2012 | Retrospective cohort study n=200 | Succinylcholine 1.7 ± 0.7 mg/kg vs Rocuronium 1.3 ± 0.4 mg/kg | After intubation, 77.5% (n=155) of patients were initiated on a sedative infusion of propofol (n=148) or midazolam (n=7). Mean time to post-intubation sedation was significantly greater with rocuronium compared to succinylcholine (27 min vs 15; p <0.001) |
| Marsch, 2011 | Prospective, randomized, controlled, singleblind, single-center study n=401 | Succinylcholine (dosing not reported) vs Rocuronium (dosing not reported) | No difference in oxygen desaturations between succinylcholine and rocuronium (P = .67) |
| Magorian, 1993 | Prospective, randomized, singlecenter study n=50 | Succinylcholine or vecuronium vs rocuronium | Onset time of rocuronium 0.9 mg/kg and 1.2 mg/kg rocuronium and succinylcholine (1 mg/kg) were similar; onset times for rocuronium 0.6 mg/kg and vecuronium (0.1 mg/kg) were much longer |
Comments by ED Physician Attendings
| Pro’s | Con’s |
| ” Has reversal agent, not associated with malignant hyperthermia, not associated with hyperkalemia (no fasciculation), dosed on ideal body weight (100mg will give 1.2 mg/kg for male that is 6’4)” | ” Longer paralytic time, however has reversal agent” |
Summary
The induction is for the patients but the paralytic is for the provider!
Summary of Paralytic Agents for RSI
| Drug | Dose | Onset | Duration | Pearls |
|---|---|---|---|---|
| Succinylcholine | 1.5 mg/kg IV; 3-4 mg/ kg IM (maximum 150 mg | 10-45 seconds | 4-10 minutes | Malignant hyperthermia Hyperkalemia Patients at risk for hyperkalemia |
| Rocuronium | 1-1.2 mg/kg IV | 45-60 seconds | 30-90 minutes | Inability to mask ventilate |
| Vecuronium | 0.1-0.2 mg/kg IV | 2-4 minutes | 20-60 minutes | Potential prolonged intubation |
