Why Do We Use Induction Agents?
To ensure adequate sedation to a patient prior to paralysis and endotracheal intubation
Etomidate
Mechanism of action
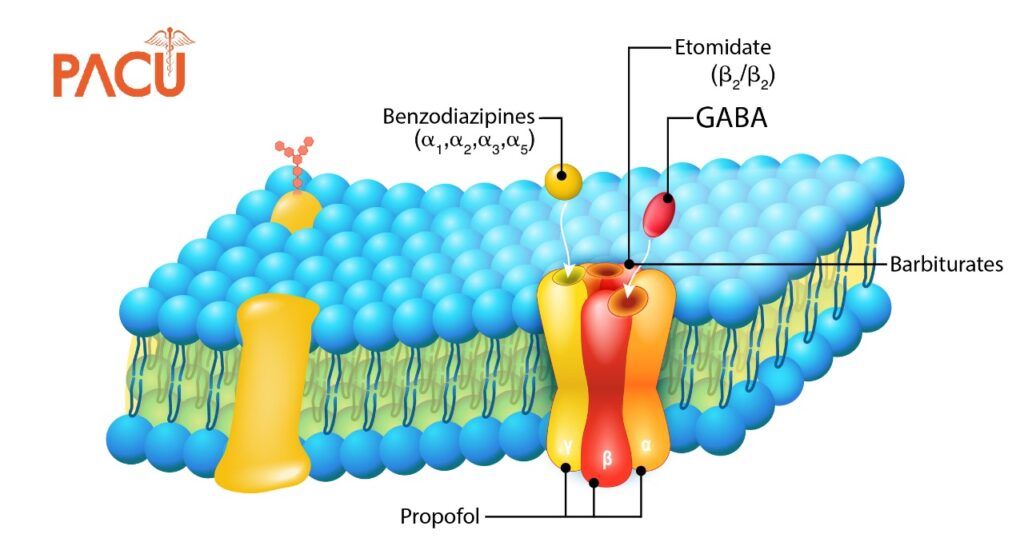
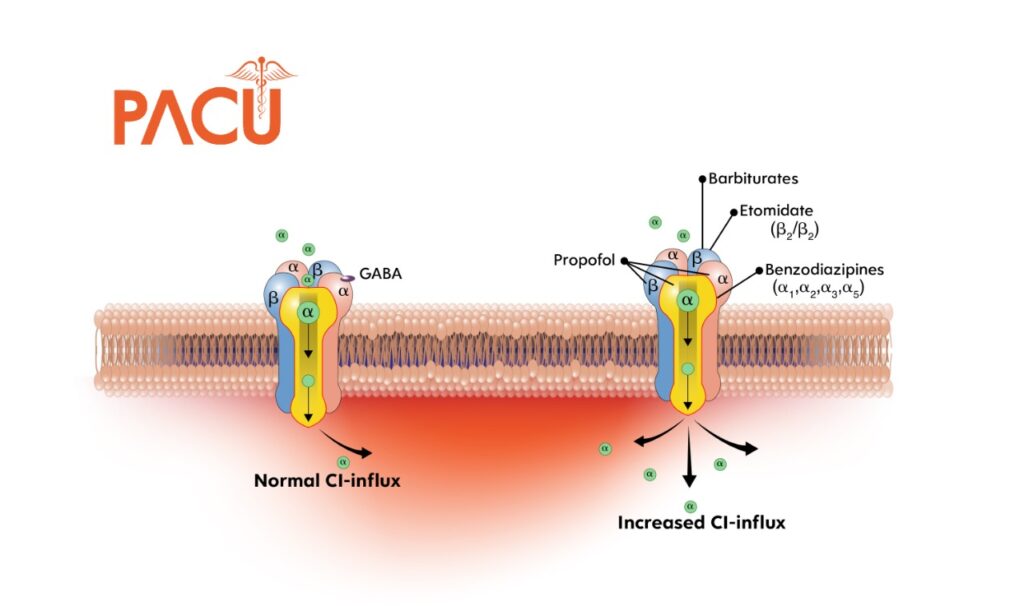
Etomidate is GABA receptor agonist that blocks neuroexcitation and induces unconsciousness.
Etomidate is imidazole-derived which is sedative-hypnotic that is a commonly used induction agent for RSI.
Dose
- The most common dose used is 0.3 mg/kg IV
- An adjusted body weight is recommended in morbidly obese patients.
Onset
- 15-45 seconds
Duration
- 3-12 minutes
Adverse effects
- Myoclonus can occur 25-63%
- Can be mistaken for seizure activity
- Pain on injection
- Thought to be due to diluent propylene glycol
- Adrenal Suppression
- Inhibits corticoneogenesis and 11β-hydroxylation which may decrease cortisol and aldosterone levels, resulting in prolonged suppression.
- Etomidate causes reduction in intraocular pressure (IOP).
Impact on Hemodynamics
| Blood Pressure (BP) | Heart Rate (HR) | Cardiac Output (CO) | Intracranial Pressure (ICP) |
|---|---|---|---|
| ↔ No Impact | ↔ No Impact | ↔ No Impact | ↓ Decrease |
Etomidate Impact on Hemodynamics
Comment
- Etomidate has no analgesic effects.
Gold standard induction agent for RSI
Literature Review
| Author, year | Design/ sample size | Intervention & Comparison | Outcome |
|---|---|---|---|
| Lyons, 2015 | Cohort study/ n=261 | Etomidate+ Succinylcholine (Group 1) vs Fentanyl+ ketamine+ rocuronium (Group 2) | Significantly better laryngeal views with fentanyl/ketamine/rocuronium group 100% first attempt intubation with fentanyl/ketamine/rocuronium group ↑ post-intubation MAP+ HR with etomidate + succinylcholine |
| Bruder, 2015 | Cochrane Review | Etomidate Midazolam Propofol Ketamine | There was no difference in mortality, hospital LOS, duration of ventilation, and duration of vasopressors Etomidate associated with ↑ ACTH and ↓ in cortisol level |
| Tekwani K, 2010 | RCT/ n=122 | Etomidate 0.3 mg/kg vs Midazolam 0.1 mg/kg | No significant differences in median hospital LOS (9.5 vs 7.3 days), ICU LOS (4.2 vs 3.1 days), In-hospital mortality ( 26% vs 43%), or ventilator days |
| Jabre P, 2009 | RCT/ n=469 | Etomidate 0.3 mg/kg vs Ketamine 2 mg/kg | No difference in intubating condition, SOFA score, 28-day mortality, Ventilator free days, vasopressor support, or GCS |
ACHT= Adrenocorticotropic hormone; GCS= Glasgow Coma; HR= Heart Rate; MAP= Mean Arterial Pressure; RCT= Randomized Controlled Trial; Scale; SOFA= Sequential Organ Failure Assessment
Ketamine
Mechanism of Action
Ketamine causes intense amnesia by inhibiting glutamine at the NMDA receptors in the thalamocortical and limbic central nervous system (CNS).
- The heart rate, blood pressure, and cardiac output increase due to the sympathetic effects of ketamine through stimulating CNS outflow.
- This leads to fewer reuptake catecholamines from outside the cell which causes a rise in these chemicals within neurons as well as between them.
Dose
1 to 2 mg/kg (common, 100-200 mg)
Onset
- Onset: ~ IV 30 seconds IM 3-4 minutes
Duration
- Duration: 5-10 minutes
Adverse Effects
- Hypertension
- Tachycardia
- Nausea & Vomitting
- Emergence phenomenon
Ketamine Impact on Hemodynamics
| Blood Pressure (BP) | Heart Rate (HR) | Cardiac Output (CO) | Intracranial Pressure (ICP) |
|---|---|---|---|
| ↑ Increased | ↑ Increased | ↑ Increased | ↔/ ↓ No Change/Decrease |
Literature Review
| Author, year | Design/ sample size | Intervention & Comparison | Outcome |
|---|---|---|---|
| Lyons, 2015 | Cohort study/ n=261 | Etomidate+ Succinylcholine (Group 1) vs Fentanyl+ ketamine+ rocuronium (Group 2) | Significantly better laryngeal views with fentanyl/ketamine/rocuronium group 100% first attempt intubation with fentanyl/ketamine/rocuronium group ↑ post-intubation MAP+ HR with etomidate + succinylcholine |
| Bruder, 2015 | Cochrane Review | Etomidate Midazolam Propofol Ketamine | There was no difference in mortality, hospital LOS, duration of ventilation, and duration of vasopressors Etomidate associated with ↑ ACTH and ↓ in cortisol level |
| Jabre P, 2009 | RCT/ n=469 | Etomidate 0.3 mg/kg vs Ketamine 2 mg/kg | No difference in intubating condition, SOFA score, 28-day mortality, Ventilator free days, vasopressor support, or GCS |
ACHT= Adrenocorticotropic hormone; GCS= Glasgow Coma; HR= Heart Rate; MAP= Mean Arterial Pressure; RCT= Randomized Controlled Trial; Scale; SOFA= Sequential Organ Failure Assessment;
Comments by ED Physician Attendings
| Pro’s | Con’s |
| “Ketamine has some bronchodilatory properties and can be useful if intubating for asthma angioedema, airway narrowing from anaphylaxis, infection or malignant processes are the typical examples.” | “The dose should be greatly reduced in shock states- most notably hypovolemic shock as it is a direct myocardial depressant. There are some case reports of cardiac arrest when full induction doses of ketamine are pushed in these patients. In those patients, I will push 10mg at a time until dissociation occurs (usually around 0.2-0.3 mg/kg in my experience).” |
Comment
- Ketamine has an analgesic effect unlike other induction agents
- Ketamine has properties that treat seizures by decreasing excitation via inhibtion of NMDA receptor
Propofol
Mechanism of Action
Propofol is a highly lipid-soluble, phenolic derivative, which is a GABA agonist and is used as an induction agent for RSI.
Dose
- 1.5-2 mg/kg IV
Kinetics
- Onset
- ~10-50 seconds
- Duration
- 3-10 minutes
Adverse effects
- Hypotension
- Bradycardia
Propofol Impact on Hemodynamics
| Blood Pressure (BP) | Heart Rate (HR) | Cardiac Output (CO) | Intracranial Pressure (ICP) |
|---|---|---|---|
| ↓ Decreased | ↓ Decreased | ↓ Decreased | ↓ Decreased |
Literature Review
| Author, year | Design/ sample size | Intervention & Comparison | Outcome |
|---|---|---|---|
| Dietrich, 2018 | Retrospective review/ n=83 | Propofol vs Non-propofol (etomidate or midazolam) | ↑ post-intubation hypotension with propofol OR 3.64 (95% CI 1.16-13.24) Similar rates of hypotension were seen among patients who received ≤2 mg/kg and those receiving >2 mg/kg No significant differences between groups in-hospital length of stay or mortality |
| Bruder, 2015 | Cochrane Review | Etomidate Midazolam Propofol Ketamine | There was no difference in mortality, hospital LOS, duration of ventilation, and duration of vasopressors Etomidate associated with ↑ ACTH and ↓ in cortisol level |
Comments by ED Physician Attendings
Pro’s
- “Due to vasodilatory and anti-epileptic properties, propofol is most useful in hypertensive head bleeds and patients with status epilepticus those with enough BP to work with but titrate 10 mg at a time”
Con’s
- “Hypotension and bradycardia should be noted, especially in trauma patients”
Comment
- Propofol can reduce SBP by 20-25% for induction
Summary
Summary of Induction Agents for RSI
| Drug | Dosing | Onset | Duration | Adverse Effect |
|---|---|---|---|---|
| Etomidate | 0.3 mg/kg IV | 15-45 seconds | 4-15 minutes | Injection site pain, nausea, vomiting, myoclonus, adrenal suppression |
| Ketamine | 1-2 mg/kg IV 4-10 mg/kg IM | 30 seconds | 5-10 minutes | Hypertension, tachycardia, emergence phenomenon |
| Propofol | 1-2 mg/kg IV | 5-45 seconds | 3-10 minutes | Hypotension, bradycardia |
| Midazolam | 0.1-0.3 mg/kg IV | 60-90 seconds | 15-30 min | Respiratory depression, apnea, and hypotension |
Hemodynamics of Common Induction Agents
| Drug | Hemodynamic Effect | Comments |
|---|---|---|
| Etomidate | ↔ BP, ↔ CO, ↔ HR, ↓ cortisol, ↔ ICP | Prolonged inhibition of steroid synthesis in the critically ill; withdrawn from a number of countries |
| Ketamine | ↑BP, ↑ HR, ↑ CO, ↔ cortisol, ↑↓ ICP | ↔ or ↑ CPP and ↔ ICP with standard anesthetic management |
| Propofol | ↓ BP, ↓ HR,↓ CO, ↔ cortisol, ↓ ICP | Hemodynamic compromise marked in elderly, ASA 3 or more or hypovolemic patients with ‘standard’ induction dose |
| Midazolam | ↓ BP, ↓ HR,↓ CO, ↔ cortisol, ↓ ICP | Mild hypotension |