- Diagnostic tools for ACS include: ECG, cardiac enzymes, and imaging studies such as cardiac CT or nuclear myocardial perfusion imaging
Risk stratification and use of appropriate diagnostic tests is essential for accurate diagnosis and timely treatment of ACS
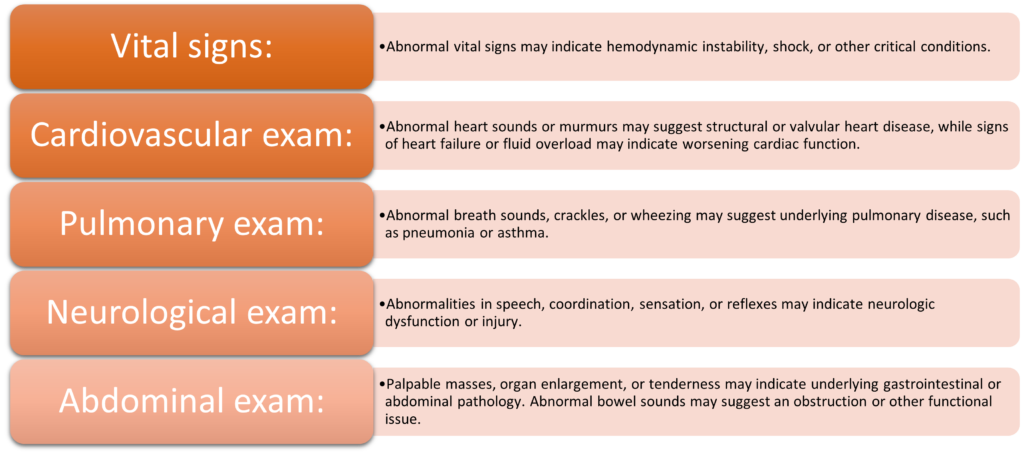
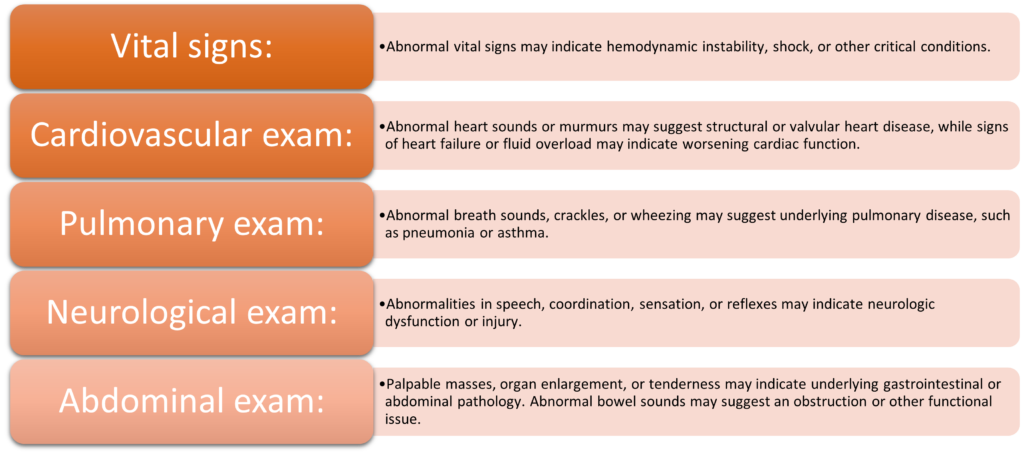
History and Physical Exam
Electrocardiography
- Provides information about the heart’s electrical activity and rhythm
- Helps identify changes associated with ischemia, injury, and infarction
- Can reveal ST segment elevation, T wave inversions, and Q waves
- Should be performed as soon as possible in patients with suspected ACS
- Repeat ECGs should be obtained for dynamic ECG changes
- Serial ECGs can also be useful for monitoring response to treatment
- Can help determine the appropriate reperfusion strategy for STEMI patients
| STEMI | NSTEMI |
| Indicates | Transmural ischemia and infarction | Subendocardial ischemia and/or nontransmural infarct |
| ST segment elevation | Present | Absent |
| T wave inversions | May be present | May be present |
| Q waves | Present, indicating transmural infarction | May be present, indicating prior MI or ischemia |
| Dynamic changes | ECG changes may evolve over time | ECG changes tend to be more stable |
| Serial ECGs | Useful for monitoring response to treatment | Useful for monitoring response to treatment |
| Appropriate reperfusion strategy for STEMI patients | ECG findings help determine the appropriate reperfusion strategy for STEMI patients | ECG findings do not directly determine reperfusion strategy but can help with risk stratification and treatment planning |
Cardiac biomarkers
- Biomarkers are substances released into the bloodstream in response to myocardial cell injury or death
- Troponin is the most sensitive and specific biomarker for myocardial infarction
- Elevated troponin levels confirm the diagnosis of MI and help with risk stratification
- CK-MB is a less specific biomarker but can still be useful in some clinical scenarios
- Biomarker levels should be obtained at presentation and at 3-6 hours after symptom onset
- Serial biomarker testing can help monitor response to treatment and risk for complications
- High-sensitivity troponin assays are increasingly used for early detection and risk stratification of ACS
| Biomarker | Description | Timing | Sensitivity | Specificity | Clinical Utility |
| Troponin | Regulatory protein released during myocardial injury | Measured at presentation and repeated | High | High | Diagnosis, risk stratification, monitoring response to treatment |
| CK-MB | Enzyme released during myocardial injury | Measured at presentation and repeated | Low | Moderate | Diagnosis |
| Myoglobin | Heme protein released during myocardial injury | Measured at presentation only | Low | Low | Rule-out ACS in low-risk patients |
| BNP | Hormone secreted by the heart in response to stress or volume overload | Measured at presentation only | Low | High | Diagnosis, risk stratification, monitoring response to treatment |
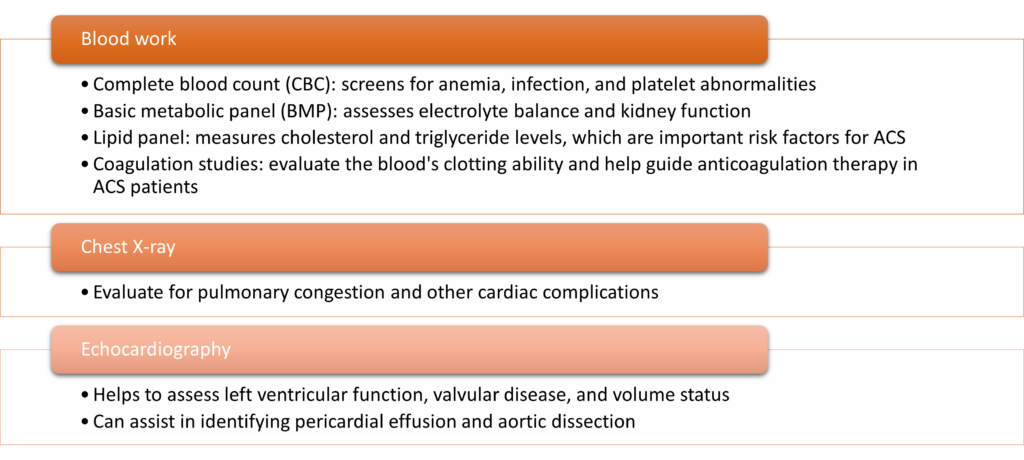
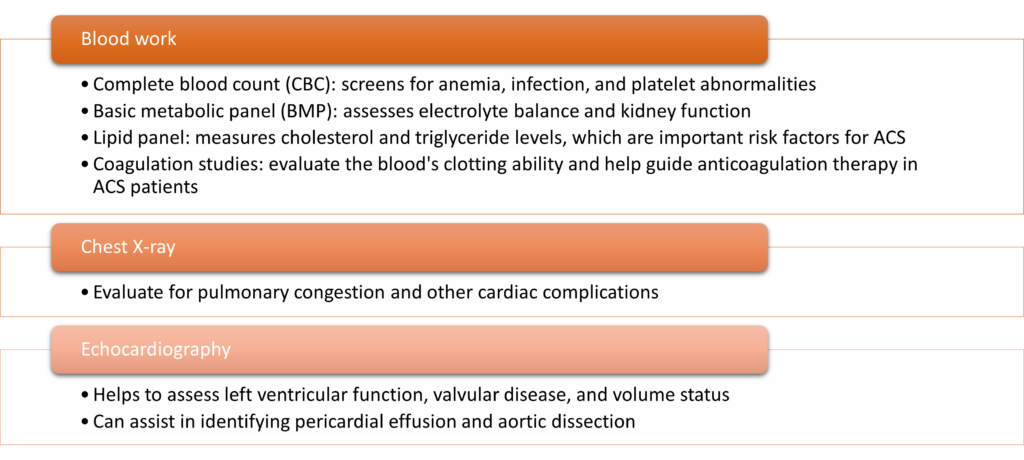
Other diagnostic tests and imaging
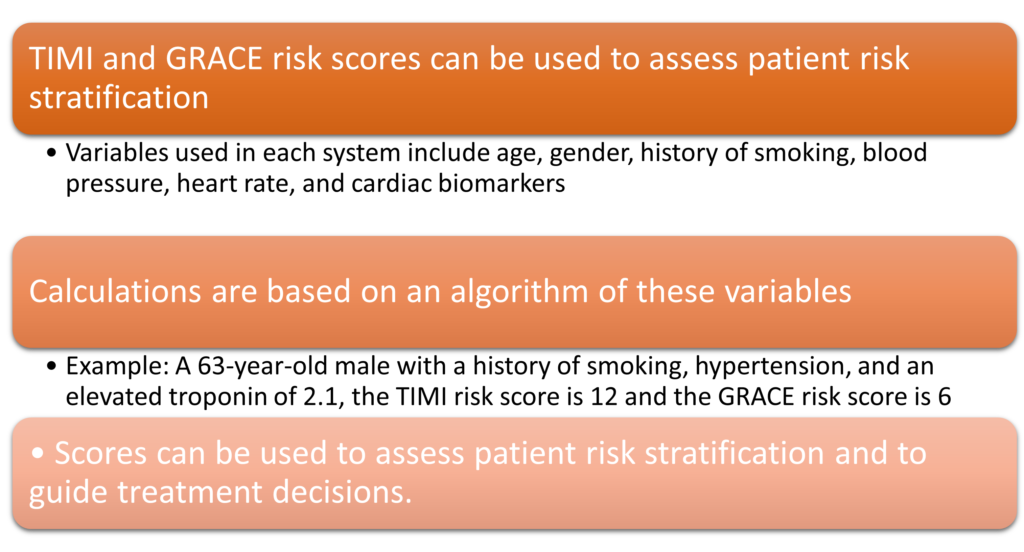
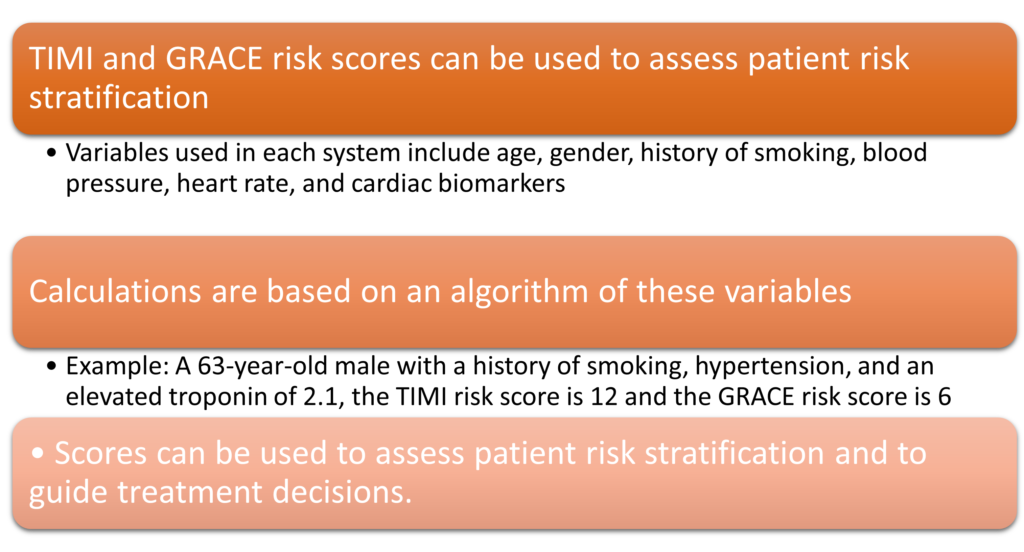
Stratification in ACS
- Multiple risk assessment tools are available for evaluating patients with ACS
- TIMI (Thrombolysis in Myocardial Infarction) score, HEART (History, Electrocardiogram, Age, Risk factors, Troponin) score, and GRACE (Global Registry of Acute Coronary Events) score are commonly used
- These tools can aid in risk stratification, guiding management decisions, and identifying patients who may benefit from more aggressive treatment
Calculating Risk Scores