Monomorphic Ventricular Tachycardia
Diagnostics for Monomorphic Ventricular Tachycardia
Monomorphic Ventricular Tachycardia (VT) is a specific type of VT where all the QRS complexes appear similar in shape on the electrocardiogram (ECG). Diagnosing monomorphic VT promptly and accurately is essential, as the arrhythmia can be life-threatening. Here are the primary diagnostic modalities and considerations:
Electrocardiogram (ECG)
- Morphology: Monomorphic VT will show wide QRS complexes (>120 milliseconds) that are consistent in morphology across the ECG.
- Rate: Typically, the heart rate during a VT episode is between 100 and 250 beats per minute.
- Absence of P Waves: P waves may not be discernible as the ventricles are activated before the atria.
- AV Dissociation: In some cases, atrial activity can be observed to be independent of ventricular activity, known as AV dissociation. This is a hallmark of VT but is not always present.
- Imaging Studies
- Echocardiogram: Helps in evaluating the structural and functional aspects of the heart. VT often arises from scarred or diseased tissue, so assessing for structural heart disease is crucial.
- Cardiac MRI: Can help identify areas of scar or fibrosis in the myocardium, which may be the source of VT.
- Laboratory Tests
- Electrolytes: Abnormal levels, especially of potassium and magnesium, can predispose to VT.
- Cardiac Enzymes: To rule out myocardial infarction as a potential trigger for VT.
In diagnosing monomorphic VT, it’s essential to differentiate it from other causes of wide QRS tachycardia, such as supraventricular tachycardia (SVT) with aberrancy or antidromic AV reentrant tachycardia.

Diagnostics for Polymorphic Ventricular Tachycardia
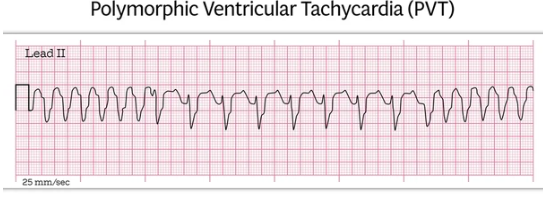
Polymorphic Ventricular Tachycardia (PVT) is a life-threatening arrhythmia characterized by varying QRS complex morphologies on the electrocardiogram (ECG). The most well-known subtype is Torsades de Pointes, which often occurs in the setting of prolonged QT intervals. Accurate and rapid diagnosis is crucial for initiating appropriate management. Here are the primary diagnostic tools and considerations for PVT:
- Electrocardiogram (ECG)
- Morphology: PVT will display QRS complexes of varying shapes, with a twisting pattern around the baseline in the case of Torsades de Pointes.
- Rate: The ventricular rate during a PVT episode typically ranges between 160 and 240 beats per minute.
- QT Interval: Evaluation of the preceding QT interval is vital, especially if prolonged, which can predispose to Torsades de Pointes.
- Absence of P Waves: Atrial activity is typically not discernible during episodes of PVT.
- Imaging Studies
- Echocardiogram: Essential for evaluating the structural integrity of the heart, as PVT can be associated with structural heart diseases.
- Cardiac MRI: Provides detailed imagery and can identify areas of scar or fibrosis in the heart muscle.
- Laboratory Tests
- Electrolytes: It’s crucial to assess levels of potassium, magnesium, and calcium. Abnormal levels can predispose to PVT.
- Medication Levels: Some medications, especially antiarrhythmics and certain antibiotics, can lead to prolonged QT intervals and predispose to PVT. Monitoring therapeutic drug levels can be beneficial.
Distinguishing PVT from other forms of ventricular tachycardia is essential because the management strategies can differ significantly. Immediate medical attention is required for anyone suspected of having PVT, and the underlying cause or trigger must be identified and addressed.
Monomorphic Ventricular Tachycardia (VT) is a specific type of VT where all the QRS complexes appear similar in shape on the electrocardiogram (ECG). Diagnosing monomorphic VT promptly and accurately is essential, as the arrhythmia can be life-threatening. Here are the primary diagnostic modalities and considerations:
Similarities:
- Both originate from the ventricles
- Wide QRS complex (>120 ms)
- Potentially unstable depending on rate and duration
- Risk of deteriorating to ventricular fibrillation
Differences:
- Monomorphic VT has a regular rhythm with uniform QRS complexes suggesting a stable reentrant circuit
- Polymorphic VT has an irregular rhythm with continuously varying QRS suggesting changing activation
- Monomorphic VT is often due to scar from prior infarction
- Polymorphic VT is often due to acute ischemia, bradycardia, electrolyte imbalance, or medication effect
- Monomorphic VT management may involve IV antiarrhythmics, overdrive pacing, or catheter ablation
- Polymorphic VT management centers on identifying and correcting any trigger plus IV antiarrhythmics
- Monomorphic VT may be well tolerated if heart function is preserved
- Polymorphic VT is unstable by definition and requires prompt termination
- Monomorphic VT may be recurrent and require chronic management
- Polymorphic VT may be a one-time event if the trigger is eliminated
In summary, the regular vs irregular QRS complexes help distinguish monomorphic and polymorphic VT. Therapy differs based on the underlying mechanism and stability.
