Atrial Fibrillation
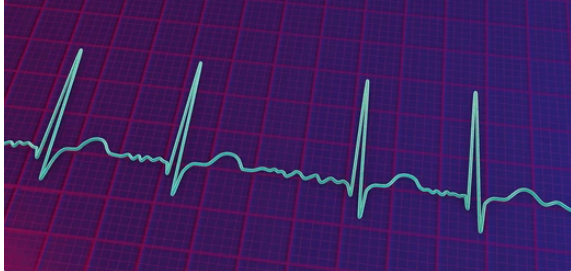
The diagnosis of AF requires documentation of the arrhythmia on ECG, which will show the characteristics of an irregularly irregular rhythm with no discernible P waves.
Additional diagnostic evaluation aims to determine the onset, type, underlying causes, and hemodynamic impact of AF. Key components include:
- History and physical exam to elicit duration and nature of symptoms, precipitating factors, medical history, cardiovascular exam findings.
- 12-lead ECG to confirm diagnosis and evaluate ventricular rate, intervals, preexcitation.
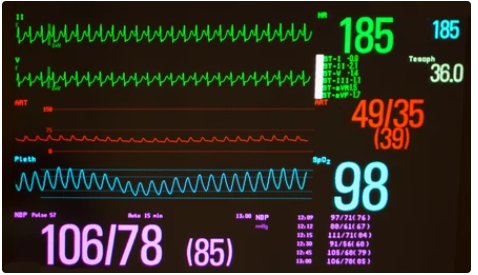
- Assessment of vital signs including heart rate and blood pressure.
- Lab tests:
- Complete blood count, electrolytes, renal function tests, thyroid function tests, cardiac enzymes and BNP to uncover contributing factors
- Coagulation studies if anticoagulation is being considered
- Chest x-ray to evaluate heart size and pulmonary congestion
- Echocardiography to evaluate chamber sizes, left ventricular function, valvular disease.
- Additional cardiac imaging (eg, CT, MRI) may be warranted in certain cases to further evaluate anatomy and function.
- Ambulatory ECG monitoring to document pattern (paroxysmal, persistent) and burden of AF
The evaluation aims to determine the type of AF (first detected, paroxysmal, persistent, long-standing persistent), identify reversible precipitating causes, assess stroke and bleeding risks using CHA2DS2-VASc and HAS-BLED scores respectively, and evaluate the need for further monitoring.
Supraventricular Tachycardia: AVNRT
ECG
On 12-lead ECG during AVNRT, the rhythm is regular with normal QRS complexes and ventricle rates typically between 140-250 bpm. The most characteristic ECG finding is RP interval (time from QRS to P wave) usually less than half the R-R interval, although not always. Retrograde P waves are typically not visible, buried in the QRS complex. Other findings may include pseudo r prime (r’) in V1, pseudo S waves in inferior leads, and pseudo Q waves in aVL. However, AVNRT ECG patterns have significant variability between patients and episodes.
Differential diagnoses to consider based on ECG include other SVTs like AVRT, atrial tachycardia, flutter or fibrillation. Adenosine can be diagnostic to help differentiate, as it will transiently block AV nodal conduction and terminate AVNRT. AVRT and atrial tachycardia will persist after adenosine.
Ambulatory Monitoring
Ambulatory ECG monitoring using Holter monitors or external loop recorders can help document tachycardia episodes. The advantage of ambulatory monitoring is ability to correlate timing of episodes with patient symptoms and activities. This can be useful in assessing frequency of recurrences, response to treatments, and triggering factors. Limitations include inconsistent patient compliance and short monitoring durations.