Lesson 1 of 6
In Progress
Background
- Clostridioides difficile (C. diff)
- Anaerobe
- Spore forming
- Gram positive bacillus
- Toxin production (A & B)
- Previously named clostridium difficile
- Renamed in 2016 in order to differentiate C. diff from other Clostridium species
- Transmitted via fecal-oral route
- Occasionally via environment

Epidemiology
- Widely present in the environment
- Asymptomatic carriers
- Infected patients
- Animals gut microbiome (canine, feline, porcine, avian)
- Large proportion of the population are carriers
- Adults:
- 3-26% in acute care settings
- 5-7% in elderly patients in long term care facilities
- < 2% in asymptomatic adults without healthcare exposure
- Adults:
- Infants:
- 15-70%
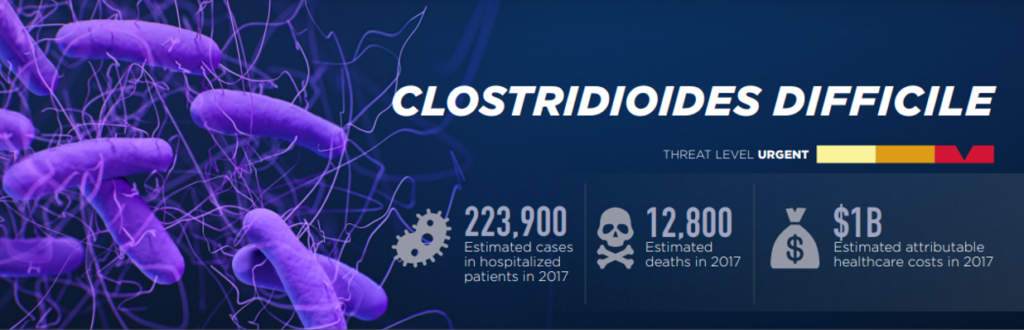
Burden of Disease
Most common healthcare-associated infection
- ~ 500,000 infections in 2017
- Incidence highest in those ≥ 65 years old
- Higher incidence in women
- Higher incidence in white individuals
- Over 2/3rds → healthcare associated
Onset – Defining Location
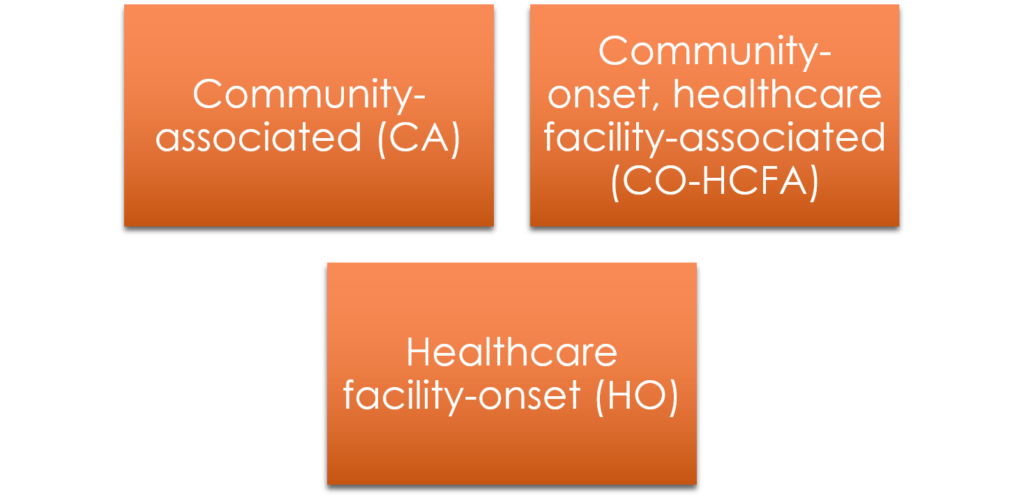
Classification
- Initial
- First Recurrence
- Second or Subsequent Recurrence
- Fulminant
Risk Factors
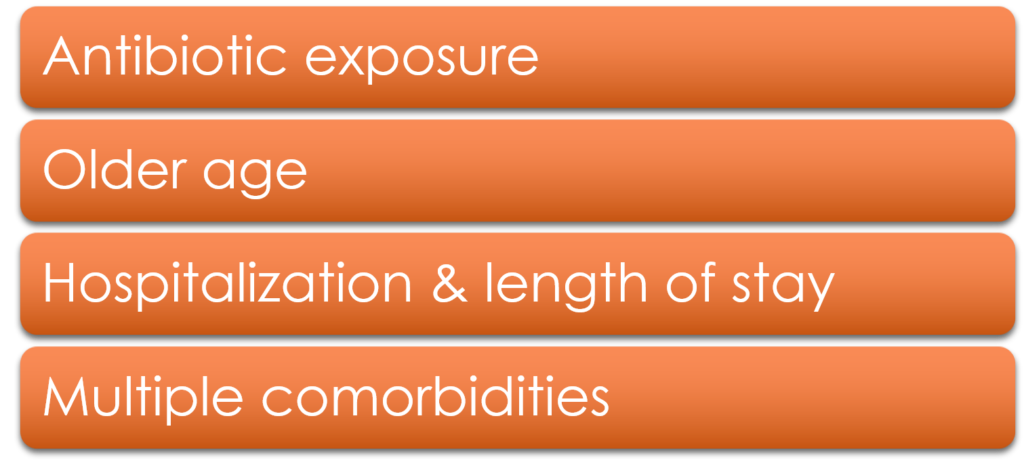
Risk Factors – Antibiotics
- Virtually all antibiotic agents have been associated with increased risk of C. diff
- Higher risk classes include:
- 3rd and 4th generation cephalosporins
- Fluoroquinolones
- Carbapenems
- Clindamycin
- Longer duration or multiple antibiotics → ↑ risk
- Risk of developing CDI increases for 3 months following antibiotic cessation (highest in 1st month)
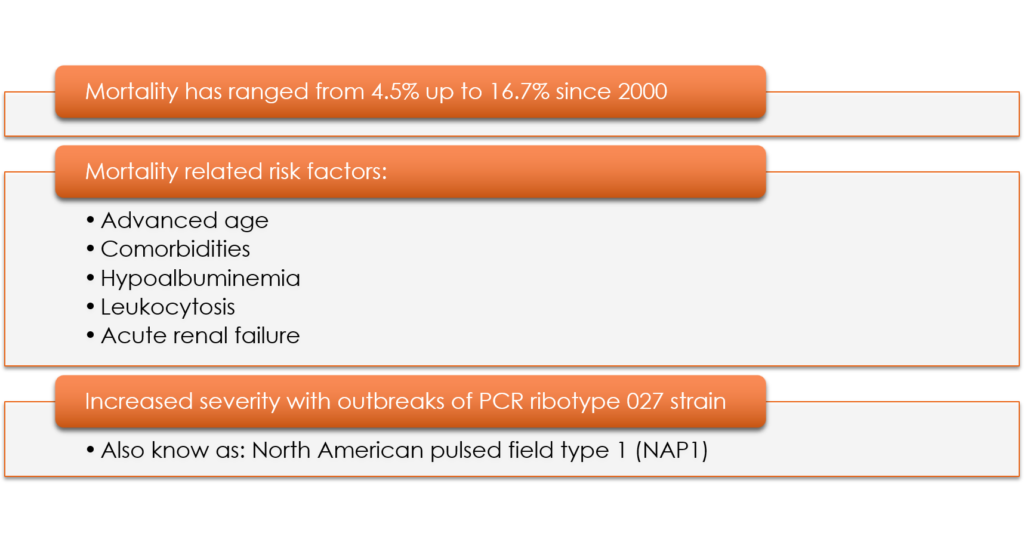
Risk Factors for Complicated Disease
- Older age
- Leukocytosis
- Renal failure
- Multiple comorbidities
- Special populations:
- Inflammatory bowel diseases
- Particularly ulcerative colitis
- Solid organ transplant recipients
- 5x greater prevalence than general medicine patients
- Hematopoietic stem cell transplants
- 9x greater prevalence
- Inflammatory bowel diseases
Risk Factors for Recurrence
- Advanced age
- Ongoing antibiotics
- Proton Pump Inhibitors
- Strain type
- Previous fluoroquinolone use
Mortality
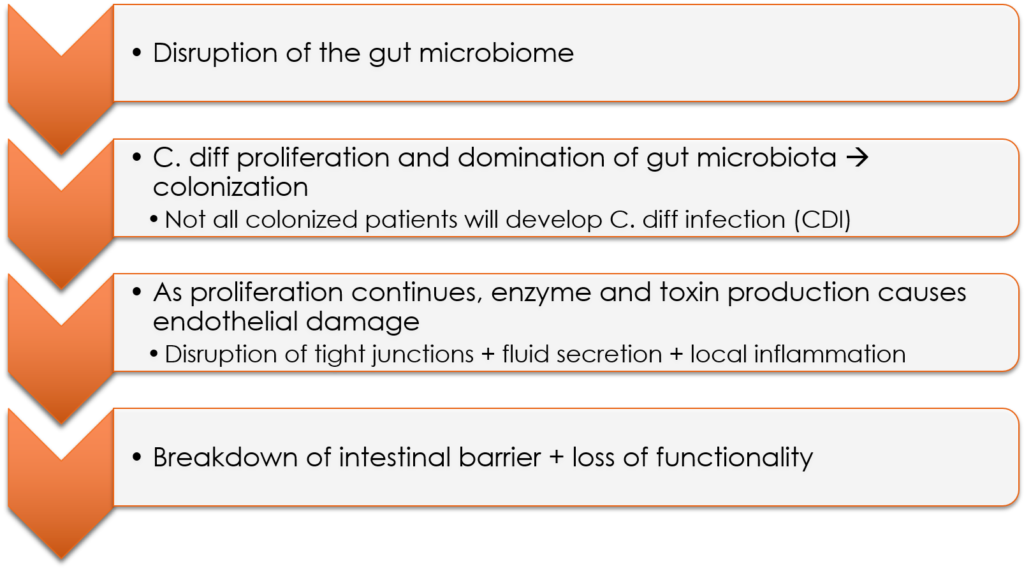
Pathogenesis
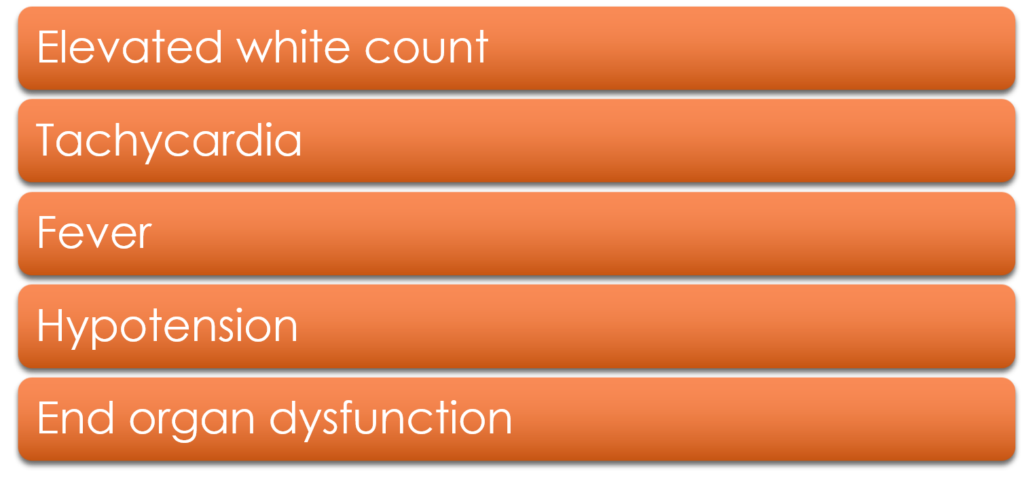
Clinical Presentation
- Large amount of variability
- Mild – Moderate – Life Threatening
- Watery diarrhea, abdominal pain, fever
Screening
- ≥ 3 unformed stools
- Within 24 hours
- Hold laxatives before testing!
Laboratory and Clinical Values
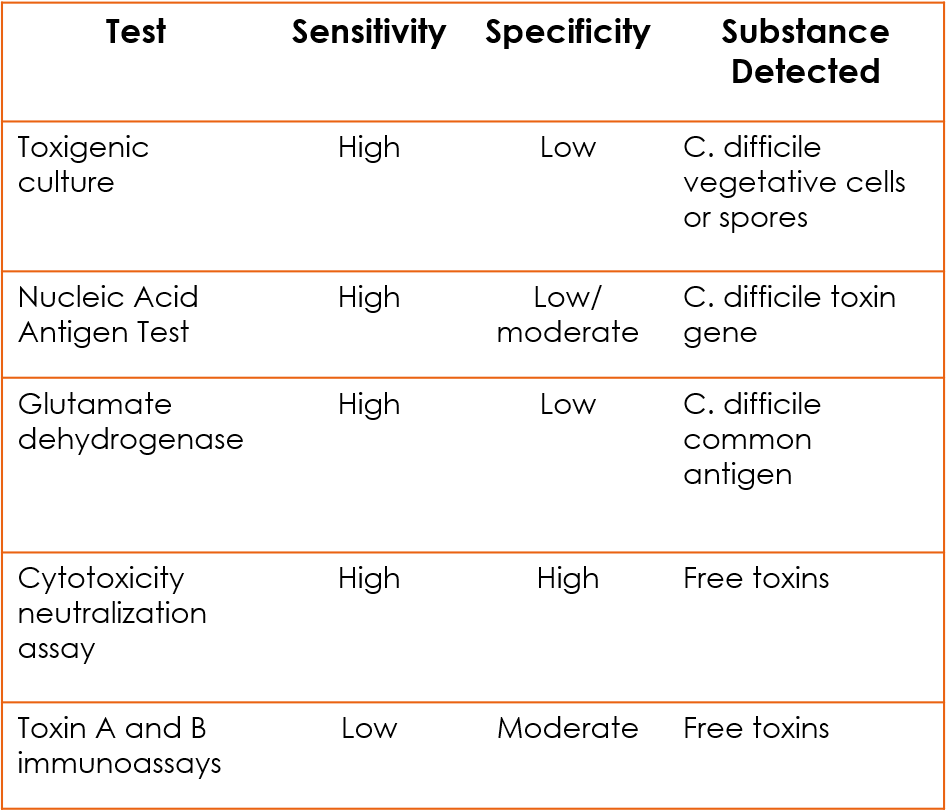
Testing
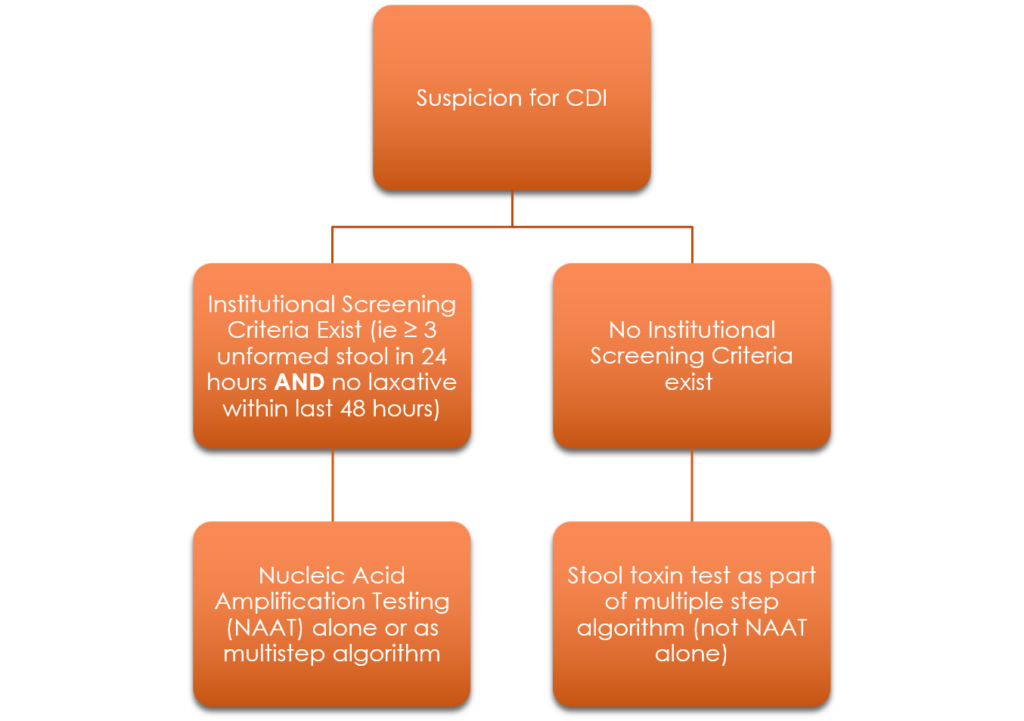
Repeat Testing
- Should NOT be performed
- During the same episode of diarrhea
- Within 7 days of initial testing
