Describe the Role that Pharmacists play in the Emergency Department
Roles and Duties of Emergency Pharmacists
Morgan et al, stated that the guidelines for EM pharmacist defined the role of the clinical pharmacist in the ED, suggested goals for pharmacy services to meet institutional needs, and established best practices.
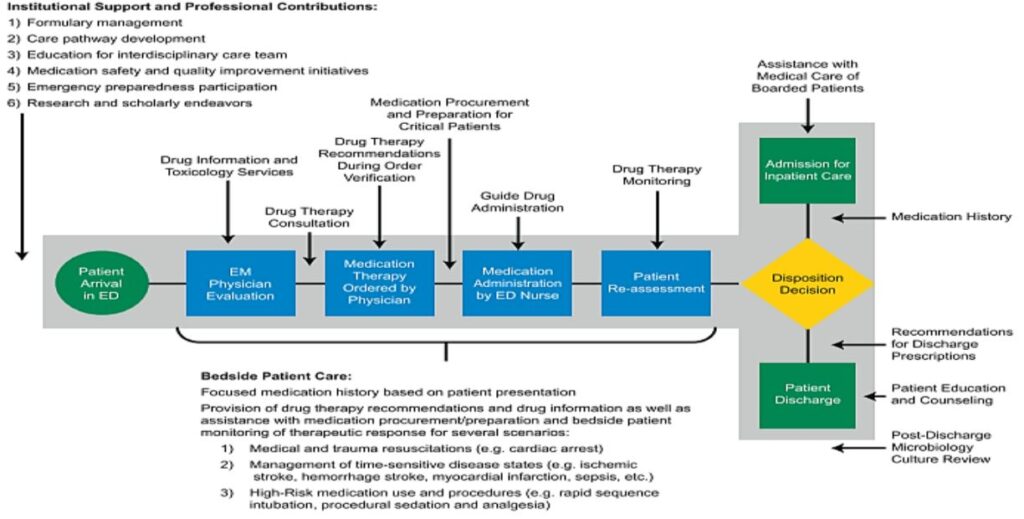
Flow of Work of Emergency Medicine Pharmacist
Pharmacist Duties in the Emergency Department
- Clinical
- Academic
- Research
- Administrative
- Distribution
- Emergency Preparedness
Current Roles and Duties of EMPs Based on the Latest Guidelines
1. Clinical Consultation
- Attend rounds and present patient information
- Dose recommendations
- Therapeutic substitution
- Disease state specific pharmacotherapy
- Pharmacokinetic

2. Clinical Duties
A. Order screening:
- Focuses on allergies, drug interactions, and appropriate dosages
B. Preparation/Selection of Medications:
- High Risk Medications
- Most appropriate medication for patient
C. Resuscitations and Trauma Response:
- During resuscitations and traumas EPh is at bedside overseeing medication use process.
The role of EMPs in resuscitation may include a variety of responsibilities including, but not limited to:
- Assisting clinicians with differential diagnosis, particularly when related to a potential medication-related cause;
- Ensuring appropriate medication selection and dose; answering medication information questions;
- Making recommendations for alternative routes of administration when appropriate; preparing medications for immediate administration;
- Ensuring appropriate administration of or administering medications pursuant to local scope of practice;
- Obtaining medications that are not readily available in the ED;
- Completing resuscitation documentation.
EPh should always be Visible and Available
- The EPh should be present at the patient’s bedside when key decisions are being made regarding medication therapy
- Dedicated to emergency department
- Physically located in emergency department
- Provided with a computer and online resources
- Easily accessible and visible to all staff with frequent “walk-through.”
- Available by pager and portable phone
3. EPh and Pediatric Patients
- Weight based dosing
- Accurate and appropriate
- Patient specific pharmacotherapy
- Medical emergency Attendance

4. EPh as an Educator
A. Patient Education
- Medication specific education
- Asthma
- Warfarin
- Low Molecular Weight Heparin
- Diabetes
- Discharge counseling
- Smoking cessation
- Over the Counter Products
- Ensure patient compliance
B. Nursing Education
- Conducts continuing education sessions
- New medications
- Drug warnings
- Drug-drug interactions
- Mock codes
- High risk medications
- Safe medication delivery
C. Healthcare Provider Education
- Provides up to date, evidenced based research on pharmacological therapy
- Develops a pharmacology elective for residents
- Becomes an established authority through education
5. EPh in Research
- Assists with research for improving patient safety in emergency medicine
- Initiates/coordinates clinical and practice based research in EM population
- Interdisciplinary EM clinical research
- Identification of patients for enrollment of investigational drug studies recruiting in the ED
- Participation in interdisciplinary research committees that review ED related research protocols
- EM related research grant preparation
- EM medical resident research projects or quality improvement projects
- Participation in articles, book chapters, case reports, or other collaborations with EM physicians
6. EPh and Quality Improvement
A. Development of clinical pathways
B. Pharmacist oversight of patient protocols
- Community Acquired Pneumonia
- Procedural Sedation
- Analgesic/Antipyretic in Pediatrics
- Febrile Neutropenia
- Acute Myocardial Infarction

Pharmacotherapy Optimization by EPh
A. The role of the emergency pharmacist in trauma resuscitation:
Pharmacotherapy of managing acutely injured patients presenting to the ED.
A working knowledge of trauma is essential given the time sensitive and the potentially chaotic nature of the resuscitation of these patients in the ED.
B. Early management of stroke in the emergency department:
- A retrospective study attempts to show that pharmacists may have a beneficial impact on the door-to-rtPA time and patient care in the emergency department.
- Intravenous alteplase or recombinant tissue plasminogen activator (rtPA) has been shown to provide neurological improvement and better outcomes if administered early to ischemic stroke patients.
C. Toxicology:
- Pharmacist guidance is required in regards to both managing various toxicologic emergencies (regarding preferred antidote, dosing, and timeliness) as well as antidote stocking in hospitals.
- EPh clinical bedside presence is necessary for assessment, important clinical considerations in, and management of patients who presents with a suspected toxic ingestion.
D. Procedural sedation and analgesia in the emergency department:
- ED Pharmacists can be of great assistance in selecting and individualizing drug therapy and preventing medication errors.
- Deep levels of sedation in the ED are associated with increased mortality. Postintubation sedatives should be dose-titrated to achieve a lighter level of sedation in the ED.
Analgosedation is the preferred strategy and should be guided by validated assessment scales. These practice guidelines are particularly helpful to the EM pharmacist in advising on analgesia and sedation management in critical care.
E. Antimicrobial stewardship in the emergency department:
ED pharmacists can successfully adopt and manage such a program for patients discharged from the ED, improving not only antimicrobial therapy but patient outcomes in the ED.
The most common AS interventions in the ED are focused on clinician education or clinical decision support (or both). EM pharmacist involvement is most fully described in relation to ED culture surveillance and follow-up, prospective audit with intervention and feedback, education of EM staff, guideline and clinical pathway development, clinical decision support systems, clinical justification requirements for antimicrobials, formulary restriction, rapid diagnostic testing, shortening of duration of therapy, dose optimization, and ED antibiogram development.
