Portal Hypertension Revisited
- Increased structural resistance
- Fibrous tissue
- Vascular distortion
- Intrahepatic vasoconstriction
- Decreased nitric oxide bioavailability
- Splanchnic arterial vasodilation
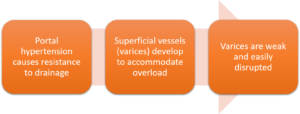
Pathophysiology
Risk of Variceal Bleed
- Varices can be categorized into high verus low risk
- High risk includes:
- Medium and large varices
- Small varices with red wale marks (indicating high risk of bleed)
- High risk includes:
Esophagogastroduodenoscopy
- Abbreviated EGD
- Identifies presence of varices
- Will also be used to identify sources of gastric bleeding
- Can be used to preemtively eliminate varices, as well as treat those that are bleeding
Primary Prevention of a Bleed
- Recommended for patients with medium/large varices at high risk for bleeding
- First line → nonselective β-blockers
- Alternative → endoscopic variceal ligation (EVL)
Primary Prevention of Variceal Hemorrhage
| Therapy | Dosing | Goals |
| Propranolol | •No ascites = Max 320 mg
•Ascites = Max 160 mg |
HR of 55-60
Stop if SBP < 90 |
| Nadolol | •No ascites = Max 160 mg
•Ascites = Max 80 mg |
HR of 55-60
Stop if SBP < 90 |
| Carvedilol | •Regardless of Ascites:
•Max = 6.25 mg BID *Unless hypertensive |
Stop if SBP < 90 |
| OR | ||
| EVL | •Every 2-8 weeks until elimination of varices | Variceal eradication |
Recap of Mechanisms
Non- selective β blockers
–β1 blockade:
-↓ cardiac output and splanchnic blood flow
–β 2 blockade:
-prevent splanchnic vasodilation mediated by β2 receptors, allowing unopposed α adrenergic effects
-↓ portal blood flow and ↑ vasoconstriction of splanchnic vascular bed
Acute Variceal Hemorrhage (VH)
- Goals:
- Control bleeding
- Maintain hemodynamic stability
- Prevent rebleed
- Prevent acute complications
Management of Acute Variceal Bleed
- Protect airway to prevent aspiration
- STAT EGD
- Blakemore/tamponade if needed
- Modest blood transfusions & fluid resuscitation
- Goal Hgb >7g/dL
- Too much can increase portal pressure, ascites, and risk of hemorrhage
- Hold inappropriate home medications
- Beta blockers
- Anti-hypertensives
- NPO if severe bleed
- Start appropriate pharmacotherapy
Pharmacotherapy for VH

Octreotide
- Local splanchnic vasoconstrictor
- Decreases blood to the variceal bleed by “clamping down” the vasculature
- Associated with lower 7-day mortality, but limited data
| Agent | Dose | Duration | Monitoring |
| Octreotide | -50 mcg bolus (can be repeated x1)
-50 mcg/hr continuous infusion |
-24-72 hours after bleeding has stopped
-Maximum 5 days |
NA |
Recap of Mechanisms
Octreotide
–↑ vasoconstriction of splanchnic bed
–↓ portal venous pressure
–↓ splachnic blood flow
Antibiotics
- With high pressure bleed → increased risk of bacterial infection
- Use of prophylactic antibiotics to prevent infection in the setting of VH
- Decreased risk of infection, recurrent hemorrhage, and death
- Given bleeding, IV route is preferred
- Antibiotics: Ceftriaxone 1g q24 hours
- Duration: Maximum of 7 days
- Ceftriaxone dosing for infection prevention (1g q24 hours) is different than that of SBP treatment (2g q24 hours)
- Once patients have recovered from a bleed, there is a need to prevent recurrent bleed
Secondary Prevention of Variceal Hemorrhage (Preventing Rebleed)
| Therapy | Dosing | Goals |
| Propranolol | •No ascites = Max 320 mg
•Ascites = Max 160 mg |
HR of 55-60
Stop if SBP < 90 |
| Nadolol | •No ascites = Max 160 mg
•Ascites = Max 80 mg |
HR of 55-60
Stop if SBP < 90 |
| WITH | ||
| EVL | •Every 1-4 weeks until elimination of varices | Variceal eradication
Prevention of VH |
The Beta Blocker Controversy in Patients with Cirrhosis
- Initially found to be beneficial, thought to decrease risk of bleed as well as rebleed after recovery from a variceal hemorrhage
- Conflicting evidence emerged in the 2000’s
-
- Are we doing harm with beta blockers in patients with cirrhosis?
-
- Piecing out the evidence
| Propranolol for prevention of recurrent gastrointestinal bleeding in patients with cirrhosis – A controlled study | |
| Design | •Randomized controlled trial
•Propranolol arm (n=38); placebo arm (n=36) |
| Population | •Cirrhosis, admitted for GI bleed and stabilized |
| Results | •Propranolol group = 96% free of recurrent GI bleed at 1 year
•Placebo group = 50% free of recurrent GI bleed at 1 year •P < 0.0001 |
| Conclusion | •Propranolol is effective in preventing recurrent GI bleeding in patients with cirrhosis |
Harm With Beta Blockers
| Author | Patients | Design | Outcome | Results |
| Serste 2010 | Refractory ascites
(n=151) |
Case-control | 1 year survival | 19% propranolol vs 64% no propranolol, NNH = 2 |
| Serste 2011 | Refractory ascites
(n=10) |
Crossover | Paracentesis induced circulatory dysfunction (PICD) | 8 patients developed PICD on propranolol, 1 patient developed PICD after propranolol discontinued |
| Mandorfer 2014 | Patients receiving paracentesis (n=607) | Retrospective | Transplant free survival | Subanalysis – patients with SBP had increased risk of death if receiving beta blocker (HR 1.58, CI 1.098-2.274) |
Benefit with Beta Blockers
| Author | Patients | Design | Outcome | Results |
| Leithead 2015 | Cirrhosis
(n=322) |
Retrospective | Mortality | Beta blockers were associated with decreased mortality in overall analysis and in subgroup analysis of patients with refractory ascites (HR 0.35, CI 0.14 to 0.86) |
| Bossen 2016 | Cirrhosis with ascites (n=1198) | Retrospective | Mortality | Beta blockers were associated with no difference in mortality in overall analysis and in subgroup analysis of patients with refractory ascites |
| Bang 2016 | Decompensated cirrhosis (n=3719) | Retrospective | Mortality | Propranolol was associated with decreased mortality when used at doses less than 160 mg/day (HR 0.7, CI 0.6-0.9) |
The Window Hypothesis
- Early Cirrhosis
- Beta blockers not indicated
- Cardiac reserve, SNS activity, and RAAS activity at baseline
- Low risk of SBP
- Decompensated Cirrhosis (Medium to Large Varices)
- BB indicated for primary and secondary prophylaxis of VH
- Decreased cardiac reserve, increased SNS and RAAS
- Increased risk of SBP
- End-Stage Cirrhosis
- BB decrease survival
- Cardiac reserve critically impaired, SNS and RAAS maximally stimulated
- Easy gut bacteria translocation
Discontinuation of Beta Blockers
- Refractory ascites
- Systolic BP < 100 mmHg
- Mean arterial pressure ≤ 82 mmHg
- Serum sodium < 120 mEq
- Severe alcoholic hepatitis
- AKI
- HRS
- SBP
- Sepsis
- Poor follow up or nonadherence
