Late 1800s to Early 1900s
- In 1874, physiologist Paolo Pellacani was the first recorded researcher to administer adrenal extract to animals. Using dogs as his subjects, Pellacani found that dogs receiving adrenal extract experienced an increase in arterial tone and blood pressure.
- His findings were soon proven by another physiologist, Rudolf Ludwig Karl Virchow Gottlieb — who induced hypotension in dogs and later used adrenal extract to restore normal blood pressure and circulation.
- Epinephrine used in resuscitation is first research by Crile and Dolley in 1906, who noted the importance of an adequate aortic diastolic pressure during attempted cardiac resuscitation. They stated that it often was not possible to achieve an adequate aortic diastolic pressure with chest compression along and needed the addition of epinephrine.

“When about a quarter of fluid has passed into the blood vessels, 15–30 minims of a one to one thousands adrenaline solution are injected into the vessel.”
— George W. Crile, Physician
Mid-1900s
- In the 1960’s, when cardiopulmonary resuscitation was still in its infancy, John W. Pearson and W. P. James Redding published a study that looked at the effectiveness of epinephrine, isoproterenol, or α-agonist methoxamine. Pearson and Redding demonstrated that epinephrine and methoxamine, but not isoproterenol, was able to restore cardiac activity in 9 out 10 dogs after asphyxiation.
- Epinephrine was in the 1974 Standards for Cardiopulmonary Resuscitation and Emergency Cardiac Care guidelines behind sodium bicaebonate.
A dose of 0.5 ml of a 1:1000 solution diluted to 10 ml, or 5 ml of a 1:10,000, should be administered intravenuously every five minutes during resuscitation effort.”
1974 CPR Guidelines
Late 1990- Early 2000s
- The 1992 ACLS gudieslines recommended either escalating doses (1, 3, 5 mg), intermediate doses (5 mg per dose rather than 1 mg), or high doses based on body weight (0.1 mg/kg).
- Epinephrine was studied at doses as high as 15 mg of epinephrine
- The overall conclusion is that it’s no better than standard 1 mg with a potential for harm based on secondary outcomes.
In 2015, the ACLS Guidelines changed it recommendation to Class III: No Benefit, LOE B-R, indicating that it did not recommend high-dose epinephrine
2015 ACLS Guidelines
Rationale For Epinephrine
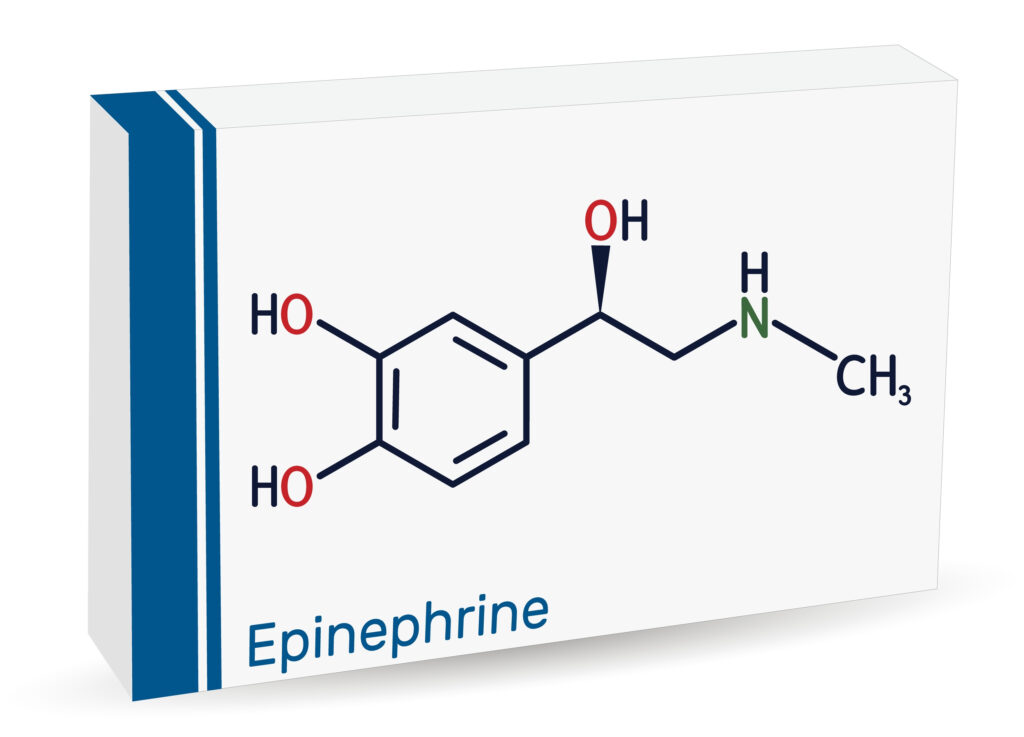
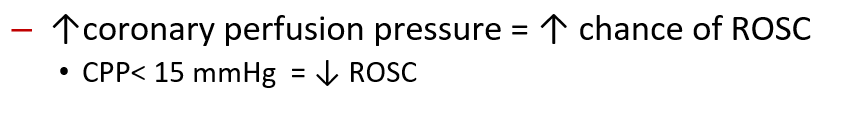
- Epinephrine increases arterial blood pressure and coronary perfusion during CPR via alpha-1-adrenoceptor agonist effects.
- Vasopressors like epinephrine assist efforts by chest compression to increase coronary blood flow
Mechanism of Action of Vasopressors
| Agent | A1 | B1 | B2 | DA | V1 + V2 |
| Dopamine | +++ | ++++ | ++ | ++++ | – |
| Epinephrine | ++++ | ++++ | +++ | – | – |
| Norepinephrine | +++++ | +++ | ++ | – | – |
| Phenylephrine | +++++ | – | – | – | – |
| Vasopressin | – | – | – | +++++ | |
| Dobutamine | + | ++++ | ++ | – | – |
| Isoproterenol | – | +++++ | +++++ |
Epinephrine Mechanism of Action
- Alpha1
- Arterial vasoconstriction
- Venous vasoconstriction
- Coronary vasoconstriction
- ↑ Cerebral constriction
- Alpha2
- Venous vasoconstriction
- Beta1 + Beta2
- ↑ Inotropy
- ↑ Oxygen demand
- ↑ Recurrent VF
- ↑ Clotting
Overall, epinephrines impact appears to be that the Alpha receptor agonism lead to ↑ SVR = ↑ CPP + ↑ oxygen delivery
Pharmacokinetics
- Onset
- < 5 minutes
- Duration
- 5-10 minutes
- Metabolism
- Extensive hepatic metabolism
- Excretion
- Mostly excreted renally as inactivated compounds
- Half Life:
- Less than 5 minutes
Adverse Effects of Epinephrine
- Epinephrine’s β-1 receptor agonism can cause a positive chronotropic and inotropic response which increases myocardial oxygen demand, resulting in complications such asmyocardial ischemia or arrhythmias.
The Dose of Epinephrine
- The dose of epinephrine used in cardiac arrest has been debated and studied for over 100 years. One of the earliest dosages recorded in modern history was of George Crile in 1906.
When about a quarter of fluid has passed into the blood vessels, 15–30 minims of a one to one thousands adrenaline solution are injected into the vessel
George W. Crile 1906
- Throughout the early to mid-1900s, many surgeons pioneers the use of intracardiac epinephrine using doses of 1-3 mg.
- The 1974 Standards for Cardiopulmonary Resuscitation and Emergency Cardiac Care Guideline recommended using an “intravenous dose of 0.5 ml of a 1:1000 solution diluted to 10 ml, or 5 ml of a 1:10,000 solution” which was extrapolated from data from intracardiac data
- Then the dose moved to 0.5 mg – 1 mg in the 1980 updated guidelines and stayed at the same until the 1992 update.
- Between the guidelines from 1980 to 1992, intense research on dosing of epinephrine was under place with many wondering of the optimal weight-based dosing.
A higher dose of epinephrine (5 mg or approximately 0.1mg/kg) is a Class lib recommendation and should be considered only after the 1-mg dose has failed.
Use of higher-dose epinephrine is acceptable but can be neither recommended nor discouraged. It is also recommended that personnel administer subsequent doses of epinephrine only 3 to 5 minutes apart rather than the previously recommended 5-minute interval
1992 Guidelines for cardiopulmonary resuscitation and emergency cardiac care. Part III. Adult advanced cardiac life support
- In the follow 2000 Guidelines, they deemphasis this practice by stating the “high-dose epinephrine is not recommended for routine use but can be considered if 1-mg doses fail (Class Indeterminate. Interpretation: acceptable but not recommended)”.
- Since 2000, the standard dose of 1 mg every 3-5 minutes has remainded the dose recommended in the ACLS Guidelines.
