- Alcohol, or ethanol, is a psychoactive substance that produces electrical changes within the central nervous system (CNS)
- Alcohol Withdrawal Syndrome (AWS) is the result of overexcitation in the CNS after abrupt reduction or abstinence from alcohol after prolonged use
- Consequences: hyperthermia, arrhythmias, or seizures
- The National Institute of Alcohol Abuse and Alcoholism reported that more than 14 million adults have alcohol use disorder (AUD)
- More than half a million episodes of alcohol withdrawal require pharmacological treatment annually
Acute Effects | Adaptations with Prolonged Use | Response to Cessation |
| Increased CNS inhibition through binding GABA-A and ↑ hyperpolarization of the nerve membrane | Down-regulation of GABA receptors through ↓ levels of GABA in the brain and reduced GABA-receptor sensitivity | Overall ↓ CNS inhibitory capacity |
| ↓ excitation through antagonism at NMDA receptors | Up-regulation of glutamate to maintain homeostatic excitation | Overexcitation at NMDA receptors via up-regulation of glutamate |
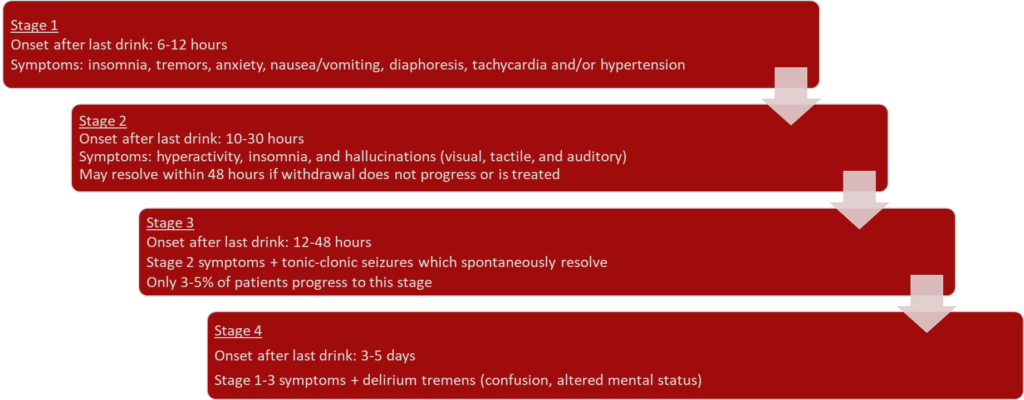
Stages of Withdrawal
•Categorized into 4 stages, which may not be sequential
DSM-5 Diagnostic Criteria for Alcohol Withdrawal
•DSM-5 is the standard diagnostic criteria for diagnosis AWS
- A.Cessation of (or reduction in) alcohol use that has been heavy and prolonged
- B.≥2 or more symptoms developing within several hours to a few days after Criterion A: autonomic hyperactivity, increased hand tremor, insomnia, N/V, hallucinations or illusions, psychomotor agitation, anxiety, generalized tonic-clonic seizures
| Diagnostic and Statistical Manual of Mental Disorders (DSM-5) Diagnostic Criteria for Alcohol Withdrawal |
| A. Cessation of (or reduction in) alcohol use that has been heavy and prolonged |
| B. Two (or more) of the following, developing within several hours to a few days after criterion A: |
| 1. Autonomic hyperactivity |
| 2. Increased hand tremor |
| 3. Insomnia |
| 4. Nausea or vomiting |
| 5. Transient visual, tactile, or auditory hallucinations or illusions |
| 6. Psychomotor agitation |
| 7. Anxiety |
| 8. Generalized tonic-clonic seizures |
CIWA-Ar
- The Clinical Institute Withdrawal Assessment for Alcohol scale in its revised version (CIWA-Ar) is the most widely used tool in US
- Used to determine the severity of the withdrawal symptoms as they are actively experienced
- Validated 10-item Assessment tool
- Examines: Agitation, anxiety, auditory disturbances, clouding of sensorium, headache, paroxysmal sweats, tactile disturbances, tremor, and visual impairment
- Score 8-15 indicates mild alcohol withdrawal
- Scores >20 indicate severe alcohol withdrawal
Saitz et al. Individualized Treatment for Alcohol Withdrawal: A Randomized Double-blind Controlled Trial
| Objective | To assess the effect of an individualized treatment regimen on the intensity and duration of medication treatment for alcohol withdrawal. |
| Design | A randomized double-blind, controlled trial |
| Setting | An inpatient detoxification unit in a Veterans Affairs medical center. |
| Intervention Control | Fixed-schedule: Chlordiazepoxide four times daily +PRNs vs Symptom triggered therapy: Chlordiazepoxide only in response to signs and symptoms of alcohol withdrawal |
| Results | The median duration of treatment in fixed-schedule 68 hr vs 9 hr in symptom-triggered group (P<.001)Mean dose 425 mg vs 100 mg (P<.001)No significant differences in the severity of withdrawal, the incidence of seizures, or delirium tremens. |
| Conclusion | Symptom-triggered therapy individualizes treatment, decreases both treatment duration and the amount of benzodiazepine used, and is as efficacious as standard fixed-schedule therapy for alcohol withdrawal. |
American Society of Addiction Medicine
- Sedative hypnotic drugs are recommended as the primary agents for managing AWD (grade A recommendation)
- There isn’t evidence that one sedative-hypnotic agent that is superior to others or that switching from one to another is helpful.
- Dose agents to achieve light sedation (grade C recommendation).
- The patient is awake but tends to fall asleep unless stimulated
- Adrenergic antagonists may be considered as adjunction (grade C recommendation)
- For control of persistent hypertension or tachycardia
